Adapted from episode 130 of The Perfect Stool podcast with Ricky Harrison, MPH, Client Engagement Coordinator at FoodMarble, developers of handheld personal devices for SIBO/IMO and food intolerance testing, and Lindsey Parsons, EdD, and edited for readability.
Lindsey:
So can you tell us about how long the FoodMarble has been around, and what are the different things it measures?
Ricky Harrison:
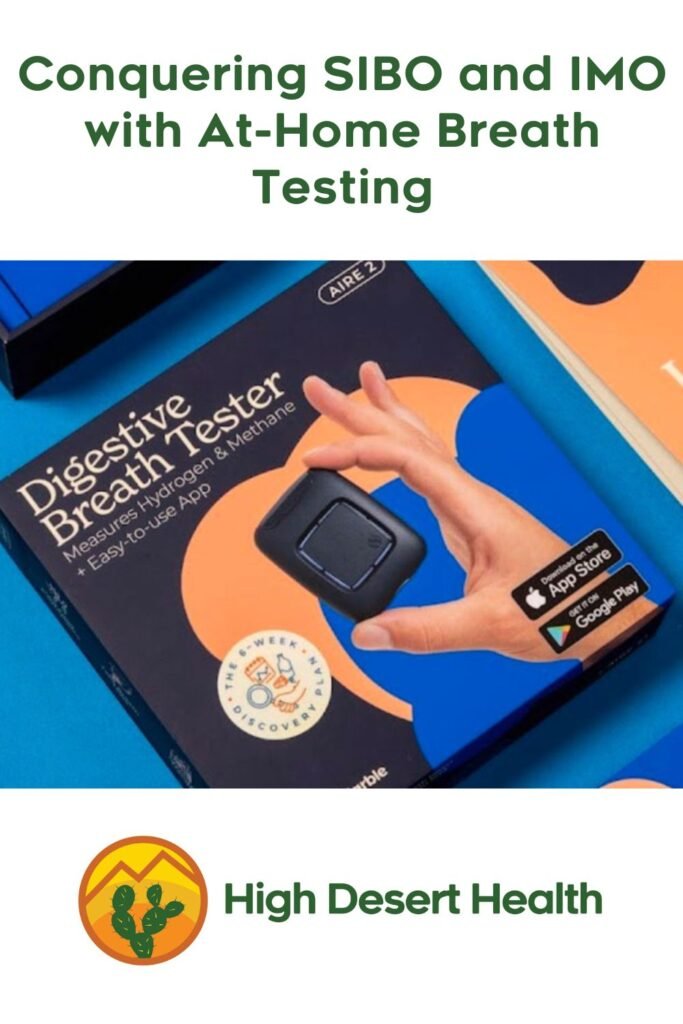
Absolutely! First we started out through crowdfunding, and that helped us with a lot of R&D and getting things set up with logistics, those types of things. So just basically getting set up and ready to start to distribute. Once we were ready to sell, we went for live sale in 2019, or I guess you could really say around November, December of 2018, so that was with our AIRE I device, and we had that going live, and we shortly released the MedAIRE device after that. And in the summer of 2022, we released AIRE 2, and MedAIRE 2 followed that.
Lindsey:
Okay, and are the med versions the medical ones?
Ricky Harrison:
Yes. So our AIRE versions are our consumer devices, and then we have our MedAIRE devices, which are FDA approved class one medical devices.
Lindsey:
And when I recommend a device to a client, are they getting the medical one?
Ricky Harrison:
Yes, so they’ll be getting MedAIRE 2, and that’s available only in the United States. The AIRE 2 and the AIRE 1 devices are still available also in the US consumer market, but that’s distributed everywhere else in the world.
Lindsey:
Cool. So I didn’t realize it was an FDA approved device. So how hard was that approval to get?
Ricky Harrison:
It was a very long, very long process, but we got there in the end. A lot of sending forms and developing various pathways for things like calibration, the way we handle complaints, all sorts of things. So it was quite involved, and that took us quite a while to get done.
Lindsey:
So do you have to prove to the FDA that you’re accurate, sensitive, and what’s the other word, specificity?
Ricky Harrison:
Yeah, yeah. We’re a completely validated machine that can produce valid results that can be used for the diagnosis of medical conditions such as SIBO, IMO, carbohydrate malabsorption, those types of things. And on the back of that, the AIRE one and MedAIRE 1 devices measure hydrogen and the AIRE two and MedAIRE 2 devices measure hydrogen and methane, and the devices can be used to either diagnose or aid in SIBO, IMO, carbohydrate malabsorption and food intolerance. (To order a medical-grade Food Marble device, the MedAIRE 2, email lindsey@highdeserthealthcoaching.com for an invitation.)
Lindsey:
Okay? And what kinds of food intolerances?
Ricky Harrison:
So we offer, currently, four different substrates for patients or customers to see how they respond to different FODMAPs. The ones that we provide currently are fructose, inulin, lactose and sorbitol.
Lindsey:
Okay. And so what are you hearing from practitioners about why they prefer the FoodMarble to laboratory SIBO and IMO testing.
Ricky Harrison:
A big part of it is having the immediate results so they can start patient treatment faster. And another thing is they are able to monitor the patient. So one of the huge advantages that we offer with FoodMarble devices, is that clinicians can follow their patients along. So let’s say a SIBO test comes back positive and they start treating the patient. They can then have the patient take daily breath tests to see how the patient is responding to treatment, how their gas profile changes as they move through the treatment. And this gives them quite a bit of information. One of them, it helps them to glean whether the treatment is working. And the second one is it allows them to see what the optimal time for retesting is. So you have a period where the patient is testing along, and their scores may be a bit higher or whatever, but over time, what you would expect to happen if the treatment is working is that the overall breath ranges will go down, and eventually they’ll level out to a point. And this gives you an idea, somewhere around this point after they’ve been leveled out for a little bit, when the optimal time for retesting is to see if you’ve cleared the SIBO.
Lindsey:
Right. So those daily breath tests are not with a substrate like glucose or lactose, and then the official tests are, correct?
Ricky Harrison:
Absolutely, yeah.
Lindsey:
And so for the regular ones, you just do it after a meal, or when would you do it?
Ricky Harrison:
So there are a couple of different ways to do it, and we’re always investigating this based on data that we’ve collected. Since 2018, millions of breath tests have been taken with the device. So we’ve lots of breath test data, lots of meal data, and we can look at all of this stuff and find out when those optimal times for breath testing are, and we’re constantly learning about that process. But the way that it would normally work is, if you have a patient and they are going through SIBO treatment, say, they can basically take one breath test an hour to 90 minutes after they’ve consumed their first meal of the day, and then they can repeat that again in the evening following their evening meal, and then that would be enough so that you can see over time, as they move through treatment, if their gas profile is going down.
Lindsey:
And why so long after a meal?
Ricky Harrison:
Well, since it’s solid food, it’s not quite as fast as the substrate. So when they are drinking the solution, that’s obviously in liquid form. It goes right down the esophagus, right through the stomach, and starts working in the small intestine. However, when you’re dealing with solid foods, that’s going to take a bit longer. It’s going to take it longer to break down in the stomach, and it’s going to take a while to eat it all. So you just want to give it a bit of time to make certain that it’s in the small intestine and then the large intestine. And then you can see how gas production is going along in those times.
Lindsey:
Okay, great. I’m glad I asked you that, because I’ve just told my clients, oh just just take it any old time to see what you get. I’m still learning how to use the device properly, as opposed to the official lab tests. And can you explain the difference between the typical testing substrates, the glucose and lactulose (and I know there’s also fructose that people are using), and what they’re recommended for?
Ricky Harrison:
Oh, yeah, absolutely. So the standard substrates for SIBO would be glucose and lactulose. And for IMO, you’re testing the small intestine and the large intestine, so lactulose is a good one for that one, because it will stay in the system from start to finish. So basically, for SIBO, you’re looking for a rise in hydrogen of 20 parts per million within 90 minutes of the test, and that’s above baseline. So if the baseline is five, you’re looking for a rise of 20 parts per million. So you’ll be looking at a minimum of 25 parts per million by 90 minutes. And for IMO, you’re looking for a rise of 10 parts per million at any time during the test. So this can be before 90 minutes, after 90 minutes, it doesn’t matter. And again, that’s based on the baseline. So if the baseline is two, you’re looking for 12, to at least reach 12.
Lindsey:
I believe I’ve been watching webinars where SIBO experts have been saying for IMO, if you’ve got a rise of five plus the symptoms, the bloating, the constipation, that that’s probably good enough.
Ricky Harrison:
Yeah, absolutely. So symptoms play a very large part in a lot of this testing. And you mentioned fructose before, so fructose has been found to be quite effective in determining whether there’s the possibility of SIBO. And quite interestingly enough, it’s been found in a study done by Dr. Hawrelak, that testing with all three substrates gives you nearly, or at 100% accuracy, in determining whether there’s the presence of SIBO, and fructose, on its own, was more effective than both lactulose and glucose in his study. So that’s also another substrate that can be used. And even working with clinicians, I’ve seen that become a more popular option.
Lindsey:
And do you use that in the same quantities you would use the glucose and the lactose?
Ricky Harrison:
So we offer it in a 25-gram sachet, which is pretty much what you’d use for fructose intolerance. So it’s the same substrate. You can use it for both.
Lindsey:
Okay, yeah, what then differentiates fructose intolerance from SIBO? And is it possible that fructose intolerance isn’t actually a thing, that it’s just SIBO?
Ricky Harrison:
So there is SIBO-induced fructose intolerance, and then there’s fructose intolerance. So SIBO-induced fructose intolerance is basically that you’re testing a patient and you’re using fructose as your substrate, and they have that initial high rise, or they have that typical rise that you’re looking for. For SIBO, in a way, you may not know it’s SIBO-induced fructose until you treat for the SIBO, and then if you test again with the fructose you may see it flattens out, and then you may see a rise at the end, which means it’s in the colon, which is normally where you would expect to see it. If it is the food intolerance, or fructose intolerance, you expect to see it after that 90 minutes, because it would be colonic at that point.
Lindsey:
Oh, okay, so fructose intolerance is normally something in the colon?
Ricky Harrison:
Typically, yes.
Lindsey:
Okay, and what about the other food intolerances? Are they measured differently than, say, on a SIBO test, like, what constitutes a positive test for the other substrates?
Ricky Harrison:
Yes. So for our food intolerance, we use the European guidelines, and so it’s really fructose and lactose. And so you’re really looking for a rise based on the European guidelines at any point during the test. So it could, in turn, be SIBO-induced fructose intolerance. So we use that for all of them. So for inulin, lactose, sorbitol, we use that guideline at any point during the test. You’re looking for a rise of 20 parts per million.
Lindsey:
Yeah. So the dilemma, of course, you know, you talked about it, yeah, if you do all three substrates (fructose, glucose and lactulose), you’ll get a perfect rating on SIBO. The dilemma is that it’s really kind of a big deal to do a breath test. And now, having just done them, I can say, right, so the day before, you have to restrict your diet to like, four foods, right? What is it, chicken, rice, eggs, a little bit of butter or oil, salt and pepper.
Ricky Harrison:
Potato. Yeah, we would definitely recommend staying away from butter unless it’s lactose free.
Lindsey:
Butter, oh, right, okay. Or ghee, ghee, I think it was, right? Okay, so you’ve already done that, so then the next day, you’ve got to wake up and drink this solution that’s full of sugar. So a lot of the people that I’m dealing with already have very sensitive guts that really don’t like sugar in any form because it’s going to cause inflammation, right? So then they have to drink this solution, and then they have to spend the next almost three hours, is it?
Ricky Harrison:
So it’s two hours if you’re using glucose, but three hours if you’re using any other substrate.
Lindsey:
Okay, so two to three hours testing every 15 to 20 minutes, depending on whose test you take.
Ricky Harrison:
Absolutely.
Lindsey:
So it’s a bit of a commitment. So, you know, you’ve got to be home, you can’t eat anything else. So the whole process is kind of cumbersome, say, compared to a stool test. So the idea of doing three different substrates to me seems kind of silly, like you want to get the most bang for your buck. It seems like the Hawrelak study showed that fructose was actually the best bang for your buck. Well, I guess there’s also the dilemma that in the US, you cannot get lactulose without a prescription. So then I’m suggesting, get your own fructose online, or whatever, if they’ve gotten the glucose kit, and then use that instead to test with right? So that just makes me think of a question I hadn’t thought of, which is, have you guys considered just sending out fructose as a testing medium, or is it just not accepted in the standards of practice yet?
Ricky Harrison:
So you can’t do that. Well, if the clinician is comfortable diagnosing SIBO using fructose, we are more than happy to provide that for the clinician.
Lindsey:
Instead of glucose?
Ricky Harrison:
Yeah, just let us know that “I use fructose, I want to use fructose,” and contact me.
Lindsey:
Oh, okay, great, great. You know, that would be wonderful, because I think I’d much rather catch more of the cases with fructose, especially because a lot of my people that I’m recommending it to are people who have the signs of methane overgrowth, of the constipation and bloating and sometimes smelly gas and such. So, yeah, yeah.
Ricky Harrison:
Back to the point of Dr. Hawrelak’s study is just the three will get you the 100% accuracy. Now fructose on his own will give you the highest of the three. He found it was around 85.7% I think it was, but you can even combine two. So in one of his interviews that I did watch some time back, he said that he stopped using glucose altogether and was just doing lactulose and fructose. And I think that gives you somewhat in the 90s of accuracy.
Lindsey:
Ah right, yeah. But again, in the US, you know, if you’re not a doctor, you can’t prescribe it, so you can’t really get it here. But okay, and then what was the percentage for glucose alone?
Ricky Harrison:
Glucose on its own, I think it was, I think it was 70 something.
Lindsey:
Okay. But so what was he testing it against? So he was saying, we know these people have SIBO. How did he know that? Because some other testing medium showed it, or because there was some other, you know, an endoscopy with a . . .
Ricky Harrison:
So one of the limitations that he did point out was that it was just the breath testing that was used. So it was a lactulose breath test on its own, a fructose breath test on its own, and a glucose fructose test.
Lindsey:
Okay, so the assumption was that if they took all three breath tests and one of them came back positive, they have SIBO. Now let’s see how they’ve done on each individual one essentially, right? Okay, so I have recommended the FoodMarble to some clients, and their biggest concern is accuracy. So I’m just curious if you have done a study of comparisons between the FoodMarble results and standard breath testing?
Ricky Harrison:
Absolutely, we’ve done several studies with research groups, some independent groups, who’ve done studies with the device as well. We do a lot of in-house studies as well, and we’ve several abstracts and papers that are available if you go to our website, foodmarble.com/GI/science. You’ll be able to see all of our studies there on the website, so you’ll be able to read them all. We have one abstract that we’re waiting to be published. We presented it at ACG, and that one goes over a validation of the hydrogen and methane against benchtop machines such as Quinton and Bedfords.
Lindsey:
Okay, so I actually did two tests at the same time. I did my test with the FoodMarble, and I did one through Aerodiagnostics that I got my doctor to order for me. And although each reading wasn’t at the exact same time, because the FoodMarble was every 15 minutes, but the other test was every 20, both came out negative for SIBO, and both showed that the only gas that went up much at all was hydrogen. So the highest point on the Aerodiagnostics for me was 16 parts per million at 80 minutes, and at 81 minutes the FoodMarble showed seven parts per million. And so I think this might be different because of the way you instruct people to breathe out without taking a breath, which is kind of tricky, because in other words you’re just barely having enough breath to finish going out, because you’re supposed to breathe out for three seconds and then put it in your mouth, and then keep breathing out. Whereas the other breath test I would breathe in, hold it a little, then I would just breathe out into the thing, so we’d get the whole thing. So I’m kind of wondering why the breathe out for three seconds then go on to the device?
Ricky Harrison:
So you’re not actually breathing out. So I have the device here, so it’s not powered on or anything, but when it’s on, all these lights will be lit up and blue all the way around. I would stop breathing and hold down this button so I’d pause my breathing, I don’t suck in or anything like that.
Lindsey:
After you’ve conceivably taken a breath, right?
Ricky Harrison:
Well, I normally, I’m just in my normal state, yeah?
Lindsey:
But I mean, you’re very conscious of whether you’ve taken a breath or not. So that’s the tricky part. You have to have enough breath to get five seconds worth of breath out. So you really have to have taken a breath.
Ricky Harrison:
Well, maybe I don’t know, but what I do, I’ll stop talking to you, and then I’ll just do it, and I’ll show you, I don’t take in a breath or anything. So I’m just now talking, and I have plenty of breath left. Okay? I do know at the start it does take quite a bit of practice, but you saw I went straight from talking to you to holding my breath; you’re really breathing for eight seconds.
Lindsey:
And what’s the concern if you actually just breathe in first, if you aren’t taking a super deep breath, but you’re just taking a normal breath?
Ricky Harrison:
Oh, you’ll be fine. The way that it works is basically, as you’re breathing through the device, you have that five second exhalation period. The actual sample is only collected at the end of that five seconds, so it’s ensuring that it’s getting alveolar breath. And so what we’re trying to do by keeping people from taking in big breaths is that they are not contaminating it with ambient air.
Lindsey:
Yeah. So okay, now I see the dilemma, because as I’m breathing out in the device, I was breathing out for three, then putting it on my lips, continuing to breathe out for five, sometimes by the end, I barely had any breath left. So that might explain why I had lower results on my FoodMarble than on my Aerodiagnostics. But most of them were pretty consistent. In fact, I was going to share this screen and show you what the two tests looked like.
Ricky Harrison:
Oh, perfect. Yeah, yeah.
Lindsey:
So this is my results from the FoodMarble MedAIRE 2. I assume I’ve got the med version, and so you see my highest reading here. Baseline was five parts per million on hydrogen, nothing on methane. And then I went up only as high as eight. So even though I had some amount of bloating, even some nausea after drinking that glucose solution, it did not show that I had SIBO. Yep. And then this was my Aerodiagnostics test. It was faxed, or whatever. You know, it’s a scan of a fax; medical systems are still in the dark ages. But anyway, this is the hydrogen column. This is the methane column. And you can see here on the chart that this is the methane down here. So I only had one at baseline and nothing else. But basically, my highest number was this 16.
Ricky Harrison:
What was your baseline? Is it 11 or 12? It looks like they’re two.
Lindsey:
I know it does look like it. Oh, it’s the combined. That’s that’s the combined line 11 of my baseline for hydrogen. Yeah, so my baseline for hydrogen here was five, whereas it was 11. So I’m sure the way I was breathing out was different. Is there a lot of hydrogen in the air? Did they get the contamination?
Ricky Harrison:
Oh, no, you’ll be fine. Well, so it doesn’t really look like they’re that far apart, though, when you think about it. So your baseline is 11.
Lindsey:
No, I mean, most of the numbers are exactly the same, like 5 6 7 6 7, same thing, 5 7 5, from baseline. I’ve only essentially gone up by five at the most here.
Ricky Harrison:
So, right. So yeah, so not terribly different at all.
Lindsey:
Yeah, tragically, I did not have SIBO, so I did not get any Rifaximin. Yeah. My original plan was actually to do the FoodMarble test determine if I had SIBO, and then if I didn’t, wait until I got it, because it always it keeps coming back for me because I have autoimmune IBS. So anyway, I did not, unfortunately, come out positive this time. So I’m having to doing the herbal supplements and control it with diet and such, which is maybe a good testament to the fact that I’m actually controlling it better than I think it is, and I’m mostly just overeating, and that’s why I’m bloating every time I go out to dinner.
Ricky Harrison:
And I’d like to point out, here’s another benefit to the FoodMarble is that you now have your device. If you want to test again, all you need is the substrate. You don’t have to order a whole another kit.
Lindsey:
Oh yeah, no, that’s the no brainer for me, when I recommend it to clients, is that if you do two tests, and people who have IMO, they’re typically having to go through multiple rounds of herbal antimicrobials. It’s very hard to eliminate. So if you can have some sense of, okay, I know it feels like this is taking forever, but some hope along the way, well, your numbers are actually going down over time. And here we have this device that can measure it, versus I’m going to have to send you out. You’re going to have to finish up your antimicrobials, then per the protocol, by request of the company, you’re probably supposed to wait two weeks after that, or a week or something, and then you’re supposed to do the prep day, all that, send it in, then three weeks later, you have the results, and you’re supposed to continue treatment. In the meantime, they’ve probably started recurring. So I definitely prefer a model in which they can keep testing.
Ricky Harrison:
And that was one of the things that we really wanted to do, because we know it’s a huge barrier. We hosted a webinar not too long ago, and we had two clinicians who work with us, and well, they both said that having the ability, that the hurdle being removed of people, being able to take a retest, has been transformative for them. So that’s really good.
Lindsey:
Yeah. And those practitioners, I remember, I watched one of those webinars, they’re typically using it more or less, you finish treatment the next day, you do the prep diet, the next day you do the device, right?
Ricky Harrison:
Yeah, yeah.
So, I mean, they’re doing it right after treatment, so you really know, okay, right after we finish, where do you stand? So then it’s, do we do another round of treatment, or do we wait and see whether it recurs after some period of time, or that kind of thing? And of course, that’s completely up to the clinician, though. So you can do it immediately, or you can so say that a patient isn’t responding as quickly as you like. Some people can sometimes respond outside of the window of treatments, so you may want to just monitor them for an additional week, perhaps, and then you may see the drop off then. So it just gives you that power that you didn’t have before. Before it was guesswork, and now you know exactly.
Lindsey:
Yeah. And so I think it’d be helpful to clarify for people what is different about what’s measured by a SIBO breath test than what’s measured in a stool test.
Ricky Harrison:
Ah, okay, yeah, I will say that they both have their purposes. Now, a stool test is giving you more of an idea of which bacteria are present and maybe the quantities in which they are there in the colon. The issue is that what you get in a stool test is more so indicative of what’s happening in the distal colon, whereas breath testing is basically telling you what the activity of the bacteria is, whether it’s high activity of the bacteria, whether it be based on timings in the small intestine or the large intestine, and the stool is just basically telling you what’s mostly there, in a sense, in the distal colon. So they do quite different things, and you can glean different things from them, so both very useful and practical tests.
Lindsey:
Yeah. So my understanding watching Marc Pimentel webinars, who is one of the biggest researchers on SIBO, is that they’re seeing SIBO almost as an infection with certain predominant bacteria in the small intestine. And then I might see a stool test from somebody who’s got a positive SIBO test, but it does not show that that’s an overgrown bacteria. Like I think it’s typically like Klebsiella and Citrobacter and E coli are the three big ones, am I right, for hydrogen SIBO?
Ricky Harrison:
Yeah, I think so. I can’t quite recall them.
Lindsey:
Okay, but then you might not see those elevated in the stool test. So it doesn’t necessarily tell you what’s going on at all in the small intestine when you look at the stool, the colon. Now methane being different, because it’s now called IMO, intestinal methanogen overgrowth and acknowledged that it can be in any part of the intestine. So it could be in the small or in the large intestine.
Ricky Harrison:
Absolutely.
Lindsey:
So Lucy mailing recently published a blog post, again questioning whether SIBO is an accurate description of what’s going on when one has dysbiosis and the symptoms of SIBO, which for me, the big one is always bloating. Like, if there’s no bloating, I’m almost like, probably not SIBO, although I’m suspicious that there are some people who strangely, just don’t bloat, like they have SIBO, but for whatever reason, they do not have a bloaty kind of system. Whereas I’m the kind of person who has a very bloaty kind of system. So even when I don’t have SIBO, I bloat. But anyway, she was also questioning breath testing as a method of diagnosis. So any comments on that article?
Ricky Harrison:
So I thought it was a well written article. And of course, everything has its drawbacks. I mean, she even pointed out aspirate cultures, which are considered the gold standard currently, has its drawbacks. Breath testing has its drawbacks, and even qPCR has its drawbacks. The thing is that what’s great about all of this, and what’s great about science in general, is that the way that we get better is that we see where there is a drawback, and we address that drawback, and we constantly grow and yeah, there’s no denying that breath testing has its drawbacks. It does just like qPCR has its drawbacks and like anything else. So what she does in practice, or in that blog article, I think she’d said that she has largely moved to qPCR for that type of thing, which is totally fine. It’s, it’s always just up to the clinician, really.
Lindsey:
Yeah which is doing something like a GI Map* or a GI Effects* or one of those tests, right? Or, I think she also used metagenomic sequencing or shotgun sequencing too. Well, at any rate for me, it’s kind of one of these things, like, for a while I stopped saying SIBO, and I would just say dysbiosis, and then at the end of the day, I’m like, I have this thing, and it does feel like an overgrowth. It feels like I sit down to dinner with everybody, and we eat the same quantity of food, and I grow a food baby, and they eat twice as much as I can, and there’s something overgrown in there, like there’s something fermenting. And, you know, that’s what it feels like to me. So I feel like the word SIBO is accurate in my personal experience, it resonates with me.
Ricky Harrison:
Yeah, I don’t have a problem with the term SIBO. They’re not really the same, in a sense.
What, dysbiosis and SIBO?
Yeah, I don’t think they’re entirely the same. So SIBO is exactly what it says it is. It’s an overgrowth of bacteria that doesn’t normally hang out in those numbers in your small intestine, right?
Lindsey:
And dysbiosis is sort of saying the same thing, but could also be something else, could be a parasite or candida, or could be a bunch of other things.
Ricky Harrison:
Anything. Yeah, absolutely.
Lindsey:
So I’m going to get my FoodMarble, and we’re going to do a little demo of me using it, so I can show people how it’s used. (See YouTube video for demo).
Ricky Harrison:
Okay, no problem.
Lindsey:
Okay, so you start and you have to double click on it, right?
Ricky Harrison:
Right. So you just give it a quick double tap, and that’s what power’s it on. So you’ll have to wait, like, two minutes, or one minute and 40 seconds.
Lindsey:
Okay, well, in the meantime, the next piece is that you then pick up your phone, and you’ve got to have downloaded the app. And the app for the medical device is different than the other app, right? It’s the one with the green that says FoodMarble Healthcare (in Apple app store / in Google play store).
Ricky Harrison:
Yeah. It has a green icon, yeah.
Lindsey:
Okay. So then on the app, I will now show, you press this little plus button, right, to take a reading?
Ricky Harrison:
Correct.
Lindsey:
Then you choose, it has logging options, and I’m going to choose breath. So now it says it’s warming up, and it shows that I’ve got to wait till these things are all blue for me to go.
Ricky Harrison:
Correct. Okay. So the warm up feature, for anyone who wonders, why why does it take so long, is the sensors have to reach a certain temperature. So what it’s doing is it’s warming up to the temperature in which the sensors will start to function.
Lindsey:
Okay. So now holding the device, that’s the air, that’s the one you blow into.
Ricky Harrison:
Yeah, correct.
Lindsey:
Yes. So now I hold it down. I’m not actually sure that worked. The phone, oh, and it says, let’s practice. Okay, so I’ve got to practice. “Let the air mix in your lungs by pausing your breathing for three seconds without inhaling,”
Ricky Harrison:
rRght? So just like I did, I was speaking with you, and I just stopped talking and held my breath.
Lindsey:
Okay, so I’m going to hold my breath for three seconds after I breathe again, because I don’t have enough breath left.
Ricky Harrison:
Okay? And it’ll vibrate, yeah? And just keep blowing until it vibrates again.
Lindsey:
Okay, I was definitely at the end of my breath at that point. Okay, now the exciting part.
Ricky Harrison:
Yeah, so that was your practice breath.
Lindsey:
That was my practice. Now, I have to do it for real, right? Now I take a real test. Okay, definitely it was the last of my breath at that point. So now on my device, I get this reading that says low. And then I say, Okay. It says, look, there’s a little bit of methane in there. It’s always interesting to me, because I always think I have, like, no methane producers, but I know you can have methane producers in your in your mouth, but not in your gut, right?
Ricky Harrison:
You can, yeah, yeah.
Lindsey:
It says, “show more”. Oh, okay, so I got some detail under “Show More”, methane point nine, hydrogen point four, overall, 1.2 but those numbers are not the official breath testing numbers. This is on a score of what, one to 10.
Ricky Harrison:
It’s zero.
Lindsey:
Yeah, zero to 10, right? Okay. Now, what’s interesting for me, though, is that I can then go on to my FoodMarble dashboard. Let me share my screen now and choose day to day. And then I will be able to see today’s test, methane, four parts per million, and hydrogen, two parts per million. That’s really funny to me. So and then then this would be the other symptoms, if I had recorded any of those right and medications and such, which I could do by pressing that plus on the device and adding those in right? And then I could see the challenge that I did from the other day, which I already showed you in the other format. But this was the actual glucose challenge that I did. So I had more methane now than I did when I did this challenge. Oh, that’s funny. Okay. Anything else you want to say about this?
Ricky Harrison:
Well, one cool thing is say that you had a positive test here, so you see this area under the curve. So what would be cool is say that you had a positive result and then you had another test after treatment, and it was still a positive result, but the area under the curve was lower. This would give you some sense that although both tests were positive, there was some improvement, and maybe you just need a little longer on treatment or something like that. So that’s pretty handy. You can also download the report. You can add it to the patient’s EHR electronic health record. Yeah, and you can also download a PDF, and this will allow you to then play around and make graphs and charts or whatever you want, and share those with the patients as well.
Lindsey:
Right? I can download this and give it to the patient. They won’t see this.
Ricky Harrison:
So if you click the download button there, you’ll get that report that you showed before,
Lindsey:
Right? But will they get that too, or only if I give it to them?
Ricky Harrison:
You have to send that to them.
Lindsey:
Okay. So in other words, there’s a lot of advantages to going through me, if they’re my client, which would be that they’re going to get the MedAIRE device that does methane and not just hydrogen. So that’s like a huge one. And then number two, that they’re going to get the chance to get a testing substrate.
Ricky Harrison:
Correct.
Lindsey:
Or do you send out the glucose for people who just buy it on their own?
Ricky Harrison:
So if you use glucose when you add a patient, you’ll have the opportunity to select what you want them to have for testing. So you can select the food intolerance kit, you can select the glucose as well, and then you can submit that. And so what happens after that is the patient then receives an email, they agree to the privacy policy, which gives their express consent for you to be able to view their data. And then after they’ve done that, they’re taken to a payment screen, and then they’ll be able to pay for it, and we ship it directly to the patient. Now there are several different account types. You can extend discounts to your patients based on which type of account you have,
Lindsey:
Right, I think there is a 15% discount in effect for my clients. And I was just asking, though, in the direct to consumer model, are you getting the testing substrates? Are you getting glucose in the US at least.
Ricky Harrison:
Yeah, so you cannot get the glucose from the website. You have to be linked to a clinician in order to get glucose.
Lindsey:
Got it, but they can get the food intolerance kit?
Ricky Harrison:
Now in the United States, the price is lower for the food intolerance kit than if they were to purchase it from the website. So they’re getting quite a few advantages by going through the clinician.
Lindsey:
Okay, and so for the food intolerance tests, are you supposed to have a prep day as well, or can you just do those anytime?
Ricky Harrison:
Yeah, so you should prep exactly the same as you do for the SIBO test. And the reason for that is so that it’s the substrate that you’re testing and not something else. So the night before, you don’t know when you’re taking your test, the next day, you don’t know if it’s the cake or if it’s the actual substrate.
Lindsey:
Yeah, no, that was also the dilemma. I got the food intolerance test, and I had every good intention of trying everything but the but the lactose, because I don’t intend to torture myself by taking lactose, which I know I’m quite intolerant to, but I was going to do the others. But then I was like, I just had to do this whole prep day, whatever. I’m not terribly tempted to do this again. Although I have had clients say after the prep day, they’re like, I haven’t felt so well in ages because they clearly had low FODMAPs food. And whereas I’m less attentive to that on a regular basis, I mean, I think maybe naturally, I’ve fallen into choosing the foods that feel better in my body. I don’t purposefully follow a low FODMAP diet all the time.
Ricky Harrison:
Yes, low FODMAP diet isn’t something that you want to carry on for a prolonged period of time anyway.
Lindsey:
No, no. So this is the nice thing for me as a practitioner, is that you can, in fact, see right away what the results are. As soon as you’re taking the test, I can go on my screen and say, okay, you got it or you don’t, and then I can let you know what I think should be the next step. So that’s what I really like. And so how much is the device?
Ricky Harrison:
Normally, for retail, $249 is the retail price for the device in USD.
Lindsey:
It comes with the glucose? So no, so the retail price is $249 for the device, retail for the glucose is $19 USD, and that is for two sachets, for the initial test and the retest. And the food intolerance kit is $49 USD, and that includes the fructose, inulin, lactose and sorbitol.
And that’s without the discount through the practitioner, correct?
Ricky Harrison:
Yes and then with your discount, it would be 15% off of that. (To order a medical-grade Food Marble device, the MedAIRE 2, email lindsey@highdeserthealthcoaching.com for an invitation.)
Lindsey:
So they get 15% off. Yeah, okay, great. So they have 15% off of $249, plus the glucose. But if I want them to use fructose, they could just get fructose online* for probably a lot less than $20 or something, and just use that, buy a big bag of fructose, and plan to keep using it for testing over and over again.
Ricky Harrison:
Okay.
Lindsey:
Okay, wonderful. Well, any anything else that we haven’t covered that we should have?
Ricky Harrison:
I think that is pretty much everything. I would like to ask you, though, do mostly practitioners listen to your podcast, or is it just a wide range of people?
Lindsey:
I would guess that it’s mostly people who have gut health issues. That’s my experience, anyway. I’m sure there are some practitioners who listen, but I wouldn’t say that’s my primary audience.
Ricky Harrison:
So that was my only question. Okay, great. Covered everything. If you have any more questions for me, please let me know.
Lindsey:
No, I think I got it, so I’m glad to be able to demo it for people. And I did say in my intro that I got the free device in exchange for the podcast, but there’s no other concrete sponsorship other than the fact that I have the affiliate account, which is something I’ve had for a good while now. So I did just want to share about it, because honestly, I think that for me, it’s a game changer, because sending somebody out for a breath test often results in disaster. And one of the biggest disasters that it results in, and this has happened multiple times, of course, there is the triosmart test that tests for all three gasses, including the hydrogen sulfide, but I’ve had multiple times now that people have done that test. And one or two or even three, or sometimes even enough samples were invalid that the test was nullified. As a result, they had to retest. Or in some cases, it just never worked. Like I had one client who did it twice, it never worked. And I thought, you know, at the very least, if I have a hydrogen and a methane breath test that comes out negative, then I can go, oh, well, maybe this is a hydrogen sulfide person, but if I’ve got no results at all, it’s hard to do anything with it.
Ricky Harrison:
Yeah, for sure.
Lindsey:
Yeah. Anyway, okay, well, thank you so much for being here. Ricky.
Ricky Harrison:
Oh, thank you so much for having me. It was a pleasure.
If you are struggling with bloating, gas, burping, nausea, constipation, diarrhea, soft stool, acid reflux, IBS, IBD, SIBO, candida overgrowth, fatigue or migraines and want to get to the bottom of it, that’s what I help my clients with. You’re welcome to set up a free, 30-minute breakthrough session with me. We’ll talk about what you’ve been going through and I’ll tell you about my 3- and 5- appointment health coaching programs in which I recommend lab tests, educate you on what the results mean and the protocols used by doctors to fix the problems revealed. Or if you’re ready to jump in right away or can just afford one appointment at a time, you can set up an 1-hour consultation with me.

*Product and dispensary links are affiliate links for which I’ll receive a commission. Thanks for your support of the podcast by using these links. As an Amazon Associate, I earn from qualifying purchases.