Adapted from episode 124 of The Perfect Stool podcast with Dr. Tom O’Bryan, an internationally-recognized speaker and author focused on food sensitivities, environmental toxins and the development of autoimmune diseases and Lindsey Parsons, EdD, and edited for readability.
Lindsey:
Dr. O’Bryan! I’ve seen you appear on many a health summit, so I was very excited when your folks reached out to me. So welcome to the podcast!
Dr. Tom O’Bryan:
Oh thank you so much, pleasure to be with you!
Lindsey:
I know you’ve published a recent book on environmental toxins, and I would like to get there eventually, but first, I’d like to focus on autoimmunity. I often get clients reaching out and asking if I’ve worked with someone with their very precise autoimmune disease. And I usually reply something to the effect of, “Yes or no, but it doesn’t really matter, because all autoimmunity has common roots.” Would you agree with that? Or are there specific antecedents that differ by autoimmune disease?
Dr. Tom O’Bryan:
Well, there are antecedents such as a genetic vulnerability or one weak link in your chain versus another. Mrs. Patient, when you pull it, a chain always breaks at the weakest link, it’s at one end, the middle, or the other end, whether it’s your heart, your brain, your liver or your kidneys. And that’s determined by two things, your genetics, and your antecedents. And antecedents is a geek word that just means how you live your life. For example, if you eat tuna fish two or three times a week, you likely have mercury toxicity. Because most, if not all, tuna is high in mercury. And that’s an antecedent, how you live your life. That’s what determines the weak link in the chain. So when your body crosses a line of tolerance, you are going to show the symptoms, wherever the weak link in the chain is. But what’s the pull on the chain? It’s always the same, always. It’s inflammation, without exception. The Centers for Disease Control tells us that 14 of the 15 top causes of death are chronic inflammatory diseases. It’s always inflammation. And that’s what we are talking about in our upcoming event.
Lindsey:
Okay. So what signs might your body be giving you that it’s moving towards a full blown autoimmune disease?
Dr. Tom O’Bryan:
Oh, that’s a really good question. And it comes down to anytime you don’t feel well. If your body’s not working the way you want it to, something’s out of balance. And I don’t mean performing in a particular athletic event at a certain level, that’s training and how you take care of yourself. I mean when your body is not functioning at levels that you consider acceptable, there’s something out of balance. My friend, Dr. Rodney Ford, who is a pediatric gastroenterologist and allergist, triple board certified, he used to answer that question this way. He says, “Well, if you are sick, your body’s not working the way it should be”. And that means your inflammation levels are high. And wherever the weak link is in your chain, that’s where you’re going to develop your symptoms.
Lindsey:
Autoimmunity in particular? Or it could be blood sugar dysregulation say, and you could be heading towards type two diabetes, but does that necessarily mean that you might also develop an autoimmune disease?
Dr. Tom O’Bryan:
It’s most common that with our metabolic imbalances, our immune systems are activated trying to protect us. And the trigger that contributes to the metabolic imbalance that you’re referring to is always inflammation. And that inflammation is going to manifest. If you do the right testing, and there are tests where you can look at 24 different antibodies to your own tissue in one blood draw. I was part of the lab that pioneered that test back in 2010.
Lindsey:
What’s that called?
Dr. Tom O’Bryan:
The lab is Cyrex*. And the test is Array 5: Multiple Autoimmune Panel*, I think that was the name. And it’s still available. It’s a great test. And it was extremely rare and for anyone who came to see us with any health complaint that the test comes back normal. You’re looking at 24 different antibodies to your own tissue: six to your brain, three to your digestive system, four to your heart, two to your thyroid, the reproductive system, the liver. When you’re looking that comprehensively, almost always we see that someone has an auto immune mechanism going on. And those mechanisms go on for sometimes decades when you have elevated antibodies.
By definition, when you have elevated antibodies, you’re killing off more cells than you’re making. So if you have elevated antibodies to your thyroid, you’re killing off more thyroid cells than you’re making. You may feel fine right now, but you’re killing off more thyroid cells than you’re making and then eventually you will develop a thyroid imbalance set of symptoms, like cold hands and feet, hard to get up in the morning, wish you had 20 more minutes in bed, chilled most of the time, energy low, a little bit of depression, weight gain, etc. All are signs that you better check your thyroid. But it takes a while before you kill off enough tissue that you start having symptoms.
Lindsey:
Right, so, I was going to ask that, and you sort of jumped right into my next question. How long can it take for you to go from healthy to a full-blown, diagnoseable autoimmune disease?
Dr. Tom O’Bryan:
Well, I’ll give you an example from this morning. I will see on Zoom, maybe one patient every two weeks. I don’t see patients very much anymore because I’m teaching all over the world. I was in Brazil in November and Rome in December and India last month. And when I was in Brazil, someone actually came hundreds of miles. I don’t know how far their town is from Sao Paulo, but they said it was a hour and a half flight. And they came and just waited outside in the hall where I was speaking to talk to me. And I was really touched. It was a very nice mother of a seven year old boy. She said, “No one can help my son, would you please help us?” And you know, I can’t say no to something like that. I said, “Okay, contact this person on my staff and go through the paperwork, and we’ll do it.” And he was a celiac but he wasn’t getting better. And he was squeaky clean, gluten free when the family travelled. Mother also brought cooking utensils and plates and silverware to make sure there was no contamination at all.
But he wasn’t getting better. And I had published a study a couple of years ago, a 14 year old boy like that who had been to three world famous celiac centers, and no one could help, but we figured it out. We ran a bunch of tests and what we found out was that he was very high in mold metabolites. The mother had her house professionally checked and they couldn’t find any mold anywhere in the house. And they couldn’t figure it out so they started to challenge the test, “is the test right?” you know. I said “You’re welcome to do it again, but this is an extremely accurate test.” It’s very rare that the test is not right on the money, the science is clear on that. So maybe you should investigate a little bit more. And the boy was spending one day a week at his grandmother’s house for an overnight and in the wall behind the headboard in the bedroom of Grandma’s house was black mold.
Lindsey Parsons:
Oh, man.
Dr. Tom O’Bryan:
You can’t see it. It’s in the wall. So they found it. But in the midst of our testing, we had found that he has one antibody slightly elevated, which is a marker to the autoimmune disease, lupus. Now there are seven antibodies to lupus. And the literature is really clear on this. The mother just emailed me yesterday extremely worried asking “Is my son going to get lupus, he’s doing so much better.” But his blood test showed that he was elevated to the antibody of lupus. And so it took me about a half hour to write the response to her. And I was really proud to take the time to do this one on one. I started off by saying, “Dear Mrs. So and So, the concerns of a mother whose child has an abnormal blood tests are never to be ignored. So allow me to take the time to explain this to you. Most doctors don’t know this.
There are seven antibodies to lupus. But every single one of them is elevated for a minimum of five years before there’s ever a symptom. Your son has no symptoms and he has one antibody elevated. It’s 20.07 and the range is up to 20. You know, it’s not 300. And I said, There is absolutely nothing to be concerned about. If this were my son, I would put zero attention on this. Now we’ll recheck it in a few months and it should be coming down. But there is good science behind the fact that mold can trigger that antibody to lupus being elevated and your son has a mold infection.” And so I sent her the study on the mold infection and I sent her the study on the antibodies to lupus, all seven are elevated years before there’s ever a symptom and multiple years before there’s a diagnosis. And that was a paradigm-shifting study because what it showed was that you can have the elevated antibodies for years before you’ve killed off enough tissue. And that’s the mechanism. You have to be killing off the tissue before you’re going to develop an autoimmune disease. So if you have elevated thyroid antibodies, by definition they’re killing off thyroid tissue.
So I said, “just breathe easy, relax.” And she wrote back and said, “I started crying when I read your message. Thank you so very, very much for taking the time to do that.” It took me a half hour. You know, I don’t have a half hour to answer those simple questions, but I feel good that I did. What we all want to understand about autoimmunity is that the antibodies have to be elevated for years. What we have to understand about Alzheimer’s, the antibodies are elevated for 20 years before there’s ever any cognitive decline. So there’s a group of them. The test is called the Neural Zoomer Plus, it looks at 53 antibodies to the brain. This is Vibrant Wellness.
But, understand that these things have to be elevated for years! Your blood sugar has to be out of balance for years before you’re ever diagnosed with diabetes. Your pipes have to be plugging up for years before you ever have coronary artery disease. And my goal is to educate people on how do you look for the earlier markers. How do you look for the markers that say, “You got a problem here. And if this isn’t addressed, this is the path that you’re heading towards. You’re on the spectrum of developing lupus, or you’re on the spectrum of developing MS.” It doesn’t matter what the disease is, it’s that you want to identify it at the earliest stage possible.
You know, there are a lot of healthcare practitioners that claim they’re dealing with root cause and root cause medicine. And when you read what they’re writing about, or talking about, they’re talking about something or some aspect and then something to sell for it. There is no root cause to all disease. There are many causes to all disease. There’s one root mechanism, and it’s inflammation! And the Center for Disease Control tells us that 14 of the 15 top causes of death in the world today are chronic inflammatory diseases. It’s always inflammation! People need to start becoming educated on this concept; you’ll hear the world leaders talking about this.
I went to seven countries and interviewed over 60 people on this topic of inflammation. I heard Professor Yehuda Shoenfeld of Tel Aviv University in Israel. His Department of Immunology at Tel Aviv University is world famous. Twenty-six of the medical doctors who went back and got their PhD in Immunology from Tel Aviv chair departments of immunology and medical schools in hospitals around the world. They’re his students! This is the godfather! We shared the stage in Rome in December, and he said a couple of things.
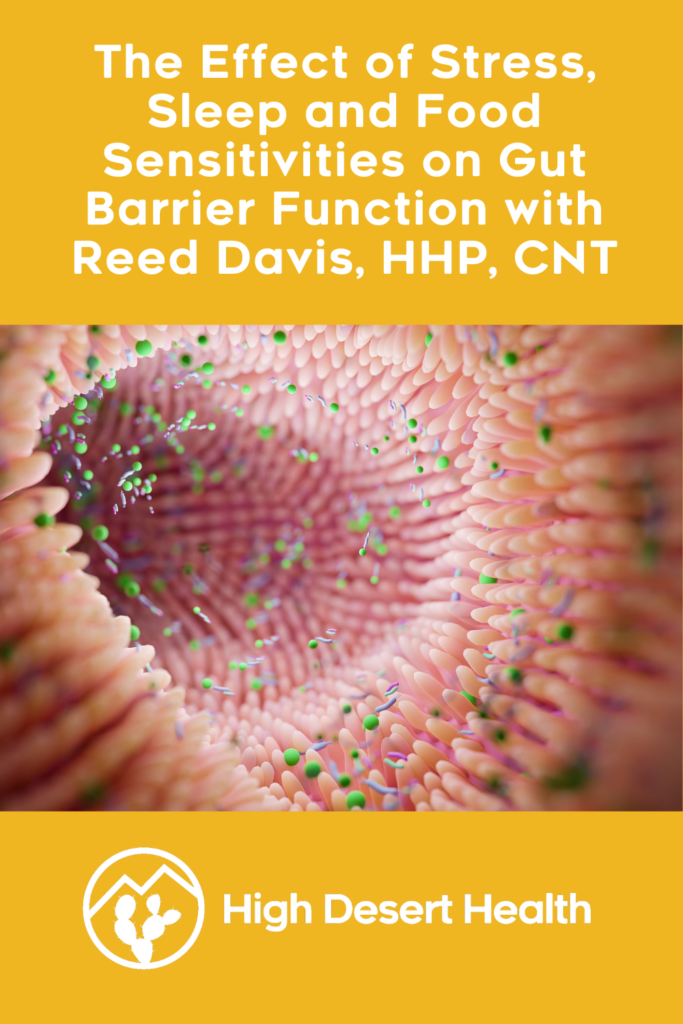
I’ll tell you two of the things that he said that were just captivating. I interviewed him afterwards for this documentary series that we’re doing. He said, “We are born 99% human”, which means there’s just a little bit of bacteria in the gut of the newborn when they come into the world. They do get a little bit of inoculation of bacteria from Mom in utero, not much, but a little. And then the birth process coming down the canal is where they get inoculated with a lot of it. And then breast milk is the coup d’etat. You know, the icing on the cake to really inoculate the gut of babies with the good bacteria. But at birth, we have about 1% of the body. The number of cells are bacterial cells. And many of us have heard that there’s 10 times more cells in the human adult of bacteria than human cells, the ratio is 10 to one.
So Schonfeld said, “We are born 99% human, and we die 90% microbial. There’s 10 times more cells of bacteria in the body than human cells. We are 90% microbial, and nobody thinks about that.” So I asked him, “Professor, you made the comment. We’re born 99% human and we die 90% microbial?” “Yes.” “Well, then, does that mean that this is really the dance of life, being how humans interact with bacteria to determine their joy of life, their function, their vitality. It all really is this dance between the bacteria in our gut and how our bodies function?” He said, “Precisely.” “
And, as an example, 36% of all the small molecules in the healthy bloodstream are the metabolites of the bacteria in your gut like short chain fatty acids, nucleic acids, DNA, etc., so are they the exhaust of the bacteria? Can I use that term for our audience? They’re the exhaust?” And Dr. Schonfeld said, “Well, yes.” I said, “You know, for example, Professor, if I exercise too hard, and my muscles are sore the next day, so I’ve got lactic acid accumulating in the muscles. That’s the exhaust of a muscle cell.” “Yes.” “And I know I just need to drink some water and in a day or two, the soreness will be gone.” “Yes.” “So are we talking about the exhaust of the bacteria in the gut that get into the bloodstream and make up 36% of the molecules?” “Well, yes, you could say it that way.” Remember, this is the godfather of auto immunity! That’s not the language he commonly uses! But he said, “Yes, you could say it that way.”
“And then professor, I have to ask the question, why? Why would nature or the creator, however you look at it, set us up to where over a third of the molecules of the small molecules in the bloodstream are the exhaust of the bacteria in our gut? Why is that?” Dr. Schonfeld said, “They are the messengers sending direction to your entire body how to function.” “Well Professor I’d heard from Michael Gershon at Princeton, he wrote the book The Second Brain in 1999.” And Dr. Schonfeld smiled, saying, “Yes, I know, Michael well.” “But Professor he said in that book that for every one message going from the brain, telling the gut what to do, there are nine messages from the gut going up telling the brain what to do?” Dr. Schonfeld said, “Yes, that’s correct.” And I said, “Is this a primary mechanism by which that direction is coming, by the exhaust in the bloodstream. Dr. Schonfeld said, “Precisely.” I said, “So our life is a dance with our gut. And when you have a bad gut, when you’ve got too many bad guys and not enough good guys, the exhaust of the bad guys are inflammatory. So you’re activating genes of inflammation.”
Remember like I said before, 14 of the 15 top causes of death are chronic inflammatory diseases. So if you’ve got bloating once in a while, if you got gas, if you got constipation, if you’ve got diarrhea, you’ve got an imbalanced gut! And an imbalanced gut means most likely you’re sending out more messages of inflammation from the bacteria in your gut than you are sending out messages activating genes of anti-inflammation. And it’s this chronic low grade inflammation, that is the root cause mechanism for every disease.
Lindsey:
So I know there are lab tests that measure inflammation, like the hsCRP, or the sedimentation rate. Are there other good measures that people can look at to just get a gauge on their inflammation without having to do fancy expensive tests?
Dr. Tom O’Bryan:
You bet, you bet. In a stool analysis, you can look at calprotectin, that’s a very common one. Eosinophil X is another one that you can look at. Elevated antibodies are by definition inflammatory. And so when you do a test looking at antibodies in your bloodstream you might say, “Mrs. Patient, your immune system is the armed forces in your body. It’s there to protect you. There is an Army and Navy and Air Force and Marines and a Coast Guard. We call them IgA, IgG, IgE, IgM, cytokines, they’re all different branches of the armed forces there to protect you.” So when you test and you’ve got elevated antibodies, or elevated markers of inflammation, then the million dollar question is, what is my immune system trying to protect me from? What is activating this defense posture. Understand that inflammation is not necessarily bad for you. It saves our life every day. Excessive inflammation is bad for you. So if you’re making antibodies to wheat, gluten, dairy, eggs, soy or any food, if you’re making antibodies and you’re eating that food, you’ve got elevated antibodies. They are triggering inflammation in your body, and that’s pulling on that chain. And wherever the weak link is in your chain, eventually, that’s where you’re going to manifest your symptoms.
Oh, by the way, I also said this to that mother and her son with the elevated antibody to lupus, I said, “It will take years of these elevated antibodies killing off tissue before your son ever has a symptom. Here’s the study on that. So don’t worry, you’re fine, you’re fine, it’s probably because of the mold, right?” But understanding this mechanism that her son is not about to fall into an autoimmune disease, it’s very serious. And we’ll be monitoring this to make sure it comes down to the normal range, although it’s only 0.7 above the range. I mean I get people that are 400, 600, way above the range. And her son was only at 20.7, and the range is up to 20. It’s not worth allocating your time to right now. But the point is, it is always inflammation.
Pay attention to scientists like David Furman from Stanford, who’s also at the Buck Institute. David Furman has the contract with NASA. Why are the astronauts aging so quickly in space? They found out a couple of years ago why it was. There’s no way astronauts can go to Mars ever, ever! It’s only a two and a half year flight and technology will get to where we could do that. But humans will die in space in two and a half years of old age, they age so quickly. And Furman’s team had been tasked to figure this out, and they did. It’s inflammation, excessive inflammation, at levels they’ve never seen before. But that’s what’s causing the sped up aging.
And Furman did this drawing, I know that we’re not on visual right now but if you imagine three gears that are interconnected. When one gear turns, it turns the middle gear, which then turns the third gear. And imagine the gear on the left to be lifestyle, things like food choices, your exposure to bacteria and viruses, your weight, are you obese, are you thin, your quality of sleep, the accumulation of toxic chemicals in your body, etc. That’s all different teeth on the gear on one side. And when one of them gets out of balance, it starts to turn the gear in the middle, which you could probably guess is systemic chronic inflammation. It’s the activation of your immune system that’s turning that gear to protect you from the excessive bacteria or the bad foods like French fries or whatever it should be, which then turns the gear on the right. These are things like neurodegenerative diseases, cardiovascular diseases, metabolic diseases. And it’s a beautiful drawing from Stanford of how all of this occurs.
The bottom line without exception, as far as I know, excluding unintentional injuries, everything else is the result of chronic inflammatory disease. Focus to learn more about your body and your family’s body. Do you or your family members have excess inflammation right now, irrespective of how you feel? Because you won’t feel anything for five years, 10 years, 20 years, you won’t feel it when you’re killing off tissue. So if you focus on learning how to ask that question and get the answers, you will extend your quality of life. There’s a difference between our biological age and our chronological age. And the average American today is somewhere around 76 years old, that’s the expected lifespan. But the expected healthy life span is 65. So the last 11 years of almost everyone’s life are with disabilities and on medications. And if you want to reduce that number so you’re not in a wheelchair, you’re not unable to walk up the stairs, you’ve got mobility, you’re fully functional, then you want to address this inflammation that’s killing off our cells now to maintain a healthier lifespan longer, rather than just extending lifespan with three, four or seven drugs, but having a healthy lifespan without drugs.
Lindsey:
Of course, that’s what we all want!
Dr. Tom O’Bryan:
I hope so.
Lindsey:
Yeah. If somebody does come to you already with an autoimmune disease diagnosed, what are the first steps in working with them to try and reverse that process?
Dr. Tom O’Bryan:
It’s always the same. First we explain to them, the science is really clear: you can arrest and reverse the development of autoimmune diseases, it’s really clear. But to do that you have to address lifestyle. Because it’s lifestyle where those environmental triggers have activated the immune system trying to protect you. So you have to identify, what is it in my lifestyle? So, if you go on holiday for a week and come home, you may think you have to air the house out. Yeah, it kind of smells dusk in there. No, that’s mold. And you have to have your house check for mold. If you have a sensitivity to wheat, you may think, “well, I only get a little bloating, you know, once in a while. if I eat pasta, it’s not too bad so I’m fine.” No, you’re not. You’re just not so bad yet that it doesn’t lay you up. So the key is to identify, “are you inflamed right now?” Unfortunately, most people won’t even entertain the question until they’re sick. And they’re immobilized and their symptoms have stopped them. And they’ve gone to two or three doctors who gave meds that couldn’t do it. Meds are great, if you need them, you take them, but it’s not a deficiency of the meds that caused the problem, right? You take them if you need them. But then you find out, why do I need them? What’s out of balance here?
Lindsey:
So it sounds like just interviewing somebody and talking to them about their lifestyle is an important first step. Are there tests that you think are also important for the next steps.
Dr. Tom O’Bryan:
Oh yes. The rule is test, don’t guess. If I were to put a bumper sticker on my car, I guess I would put that one on there. Test, don’t guess, because it doesn’t matter how you feel. You may think, “I feel fine.” But, It doesn’t matter how you feel. And let me give you an example of this, which is undeniable. It’s so overwhelming to people they just forget about it, because they don’t know how to hold the information. BlueCross BlueShield, published a study in February 2020 which got absolutely no press whatsoever because that’s when the virus came out. And that took over everything. They said, “We’ve got a problem here, we’ve got a real problem! In the previous four year period, there was a 407% increase in the diagnosis of Alzheimer’s. 407% in four years in the diagnosis of Alzheimer’s in 30 to 44 year olds.”
Lindsey:
Wow.
Dr. Tom O’Bryan:
That’s like, what? Why? That’s game changing. Which means that the inflammation started so much earlier in life for these 30 to 44 year olds, which was killing off brain cells, because we know it takes 20-25 years of that before you ever have a symptom. The government commission that came out in 2019 identified that, because they thought that Alzheimer’s was going to bankrupt Medicare, what are we going to do? And the report said that this inflammation is going on for 20-25 years before there’s ever a symptom. It’s elevated antibodies and other markers of inflammation in the brain, killing up brain cells. Let me give you one example. A paper came out five weeks ago that looked at microplastics and how bad microplastics are. But now the technology is available for nanoplastics, which is a billionth of a gram.
And this laser technology looked at one liter of bottled water, three different companies, one liter of bottled water, the average number of nanoplastics in those bottles was over 240,000 in one liter of water. Well, what does that mean? It means when you drink the water, you’re also drinking the plastic that gets into your bloodstream and goes right through the blood brain barrier and accumulates in your brain. Then your immune system, trying to protect you, fights this invader in your brain. Here comes the inflammation, which is trying to kill off this invader and there is collateral damage. This is because the immune system in the brain (you have four different immune systems), is the big kahuna, and it doesn’t have a pistol. It doesn’t have a laser-guided, high-powered rifle like special forces. It has bazookas. They’re called glial cells to kill anything that gets into the brain. But now you’ve got these nano plastic particles of water that are accumulating in the brain, activating the glial cells causing constant firing of glial cells. This results in collateral damage from the repetitive killing off of brain tissue. And that’s just one example of so many.
So what people have to learn first, they have to understand this concept. And then they have to learn, what are the environmental triggers in my life where I can start reducing some of these threats that my immune system gets activated against? And you know, we’ve all heard that adult women, by the time they leave the house in the morning, they’ve exposed themselves to over 120 chemicals, between their shampoos and their makeups. And for men, it’s over 80 chemicals before they leave the house, things like shaving cream, shampoo, underarm deodorant, and these chemicals, they (the companies/government) don’t have to prove they’re safe. Now, somebody out there is saying, “Yeah right doc, you’re just exaggerating?” No, no, it’s called the Toxic Substances Control Act. And exposure to a chemical at the dose that you’re exposed is toxic to humans in a 24 hour period. It’s not! And that’s how the chemical industry gets away with it! Rather, these toxins are accumulative in your body.
So give me a five year old girl that is painting her 10 little fingers and 10 little toes once a week for 25 years, and the phthalates from the chemicals used to mold plastic are in your bloodstream in four to five minutes after you apply nail polish. Well the companies say, “there’s no evidence that phthalates leaching out of nail polish into the bloodstream is toxic to humans.” That’s how they get away with this, but instead it accumulates in your body. Now give me that same girl when she’s 25 to 30, and she gets pregnant, hopefully has a healthy pregnancy and a healthy delivery. Now she has a family and she’s really excited.
In 2016 in Chicago, they looked at 326 pregnant women in the eighth month of pregnancy. And they did urine analysis looking for phthalates, the chemicals used to mold plastic. And they looked at five phthalates even though there are many, but they just looked at five including BPA. They categorize the results in fourths; the lowest amount, the next, the third and the highest. And they followed the offspring of those pregnancies for seven years. When the children turned seven years old, they did the Wechsler IQ tests on them. Not much in medicine is all or every but this was every. They compared every child whose mother was in the highest category of phthalates in urine during pregnancy to the children whose mothers were in the lowest quartile of phthalates in urine during pregnancy. Every child in the highest quartile, their IQ was seven points lower, 6.7 to 7.4 points lower, every child.
Now just go on Google and type in phthalates and neurogenesis. There come all the studies saying the higher the level of phthalates, the more inhibition on brain cell growth and development. But the companies say, “there’s no evidence that the amount of phthalates that leach into the bloodstream from nail polish is toxic to humans.” That’s how they get away with it. The government and these companies say, “there’s no evidence that the amount of phthalates that leach into food in leftover storage containers is toxic to humans.”
If you put your leftover food in a plastic container in the refrigerator, the next day the chickens got phthalates in it. Or these companies will say, “there’s no evidence that the amount of phthalates that leached out of the lid of a coffee cup from a coffee shop is toxic to humans.” But they put that lid on a hot liquid allowing the steam to condense on the underside of the lid, dripping that back down into the coffee with Bisphenol A, BPA. When you put the coffee cup up to your lips to take a drink, and the hot liquid hits the entire underside of the lid, tapering down into the opening with Bisphenol A. Even your soft contacts are loaded with Bisphenol A and even credit card receipts are loaded with Bisphenol A. If you grab a credit card receipt, within a couple of minutes your blood levels of BPA is hundreds of times higher than before you touch that receipt. So you have to learn about all these things because it’s overwhelming. But you just keep learning one thing at a time and you reduce your exposure. You should strive to create an environment in your home for you and your children and in the workplace to be as low toxic as possible. Everybody can do that. You just have to learn what to do.
Lindsey:
Yeah. So you know, I’m someone who’s aware of this stuff, and I pay attention too and try to do my best on these kinds of things. But there are always people in your life who poopoo it and who say, “my X, Y and Z person lived to be 80 or 90 and they were healthy and they use that same shampoo and they use the same whatever.” What would you say to those people?
Dr. Tom O’Bryan:
Yeah, I don’t have time for those people anymore. You know, you can lead a horse to water but you can’t force it to drink.
Lindsey:
Yeah but what if those people are using shampoo in your bathroom sometimes if you live with them…
Dr. Tom O’Bryan:
Well, that’s a very good point. So then you have your own shampoo in the bathroom. Right?
Lindsey:
I know. But you walk in the bathroom after they use it and the odors are overwhelming.
Dr. Tom O’Bryan:
That’s really important. You’re absolutely right. And that’s a difficult situation. Dr. Jeff Bland is the founder of functional medicine and in our interviews with him, he said, “Tom, a negative thought is just as potent a stimulant of your immune system producing inflammation as exposure to a virus.” And so if you’re living with negative people or negative thoughts, you might want to reevaluate. Or you’re destined to spend the rest of your life in this stuck situation. People do grow and expand, you know, it’s called “the seven year itch.” We all grow, we all expand, and there’s a new chapter to your life every seven years. And the question is, are you willing to explore a new chapter with your partner? Or are you guys living the same way you were 30 years ago, even now that the kids are gone?
Some people don’t know what to do, they don’t have anything to say. People just sit in front of the television, the thing my father used to call it the “idiot box” and you’re off in your own world, not interacting with other humans in your home. Excuse me for being direct, but this kills people. I don’t have time to try to convince someone. I will give you the information in the best analogies I can of what the world-class scientists are saying. And we’re also making the studies available. I asked each speaker, “send me five studies that you think are really important for clinicians, and the general public who’s interested to know, send me five studies.” So we have something like 80 or 90 studies that are just cutting edge on all of these topics that we’re talking about here today.
Lindsey:
So I work with people with gut health issues and autoimmune issues because those often follow. Often I do work on the gut for people, and I clean that up. And then I think, “Okay, if it’s still not working, what’s going on?” Then I usually look at questions of mold even if they’ve said they have no exposure or environmental toxins. So other than known exposures, are there tip offs, that you would recognize that says maybe there’s an environmental exposure here to some kind of an environmental toxin.
Dr. Tom O’Bryan:
You bet. There are four tests that anyone who wants to see me has to take. I don’t want to talk to them until I have some information to really help them. So those four tests are called the Wheat Zoomer, because you zoom in on the problem. And it also is the most accurate test I’ve ever seen for intestinal permeability, leaky gut. There is also the Neural Zoomer Plus, that looks at 53 markers of inflammation in the brain. The Gut Zoomer that looks at what’s in your gut, your microbiome, how much inflammation do you have and all that. And finally the Total Tox Burden. Have you accumulated heavy metals or glyphosate or toxic chemicals or mold metabolites, etc. So those are the four introductory tests that people will do that we recommend. There’s lots of testing out there you can do, but these four are highly accurate and highly sensitive.
Lindsey:
Are those Vibrant or Cyrex?
Dr. Tom O’Bryan:
They are Vibrant. The Mayo Clinic calls this technology a new era in laboratory medicine. It’s really worth taking a moment to talk about these lab tests. If I were to tell you in 1990 or 1995 that in about 30 years or so, I’m going to hold a little black box in my hand the size of a wallet. If I push on the front of it and slide my thumb a couple of times, I can tell you within five seconds that the air particulate matter in San Diego today is 84 so not exercise outside today! But in San Antonio it is 21 so it is a good day to be outside. In other words, I can tell you any information from anywhere in the world in seconds. I’ve got the Encyclopedia of the world in my hand, and it’s our iPhones. If I told you that in 1990, you would have thought I was watching too much Star Trek and that I was a bit of a nutcase. But we do that every day now and we take it for granted. The same thing has happened in laboratory medicine, but the technology that most of the laboratories are using are from the early 2000s.
The problem with that is that even though it is right seven or eight out of ten times, it’s completely wrong two or three out of 10 times. But the new technology is called silicone chip technology. And Mayo Clinic refers to it as “a new era in laboratory medicine.” And I have no association with the laboratory. I wish I had some stock in the company because they’re doing great work, but I don’t. They’re growing so fast because doctors are saying, “Oh, my God, look at these tests. These are fabulous.” And these tests are very competitively priced. So all four tests that I just told you about, are probably somewhere around $1400-1,500, something like that. But now you know the major tests. Sure, somebody can be sensitive to egg and you should do the Egg Zoomer, or the Dairy Zoomer or the Lectin Zoomer. Yeah, there’s other tests. But these four I mentioned give you such a comprehensive overview of the likely triggers for the majority of people of where their inflammation is coming from and where it’s manifesting.
Lindsey:
So I do test on my parents every year, who are in their 80s now and doing much better than all their friends. I like to take some credit for that. I’ve done the NutrEval* the last couple of years, and found that my dad had elevated mercury. And I knew that they had been eating fish I think some friend had caught, some mahi-mahi or something like that. And they had a bunch of it in their freezer, and they were going through it. And I pointed out his high mercury and started to talk about how we might address this. He just said, “everybody’s got this stuff, like is this really important?” What would you say to somebody like this?
Dr. Tom O’Bryan:
Yes, it’s really important. Yes. Say, “Dad, look at this study about mercury in the brain or this study mercury in the brain.” And this one that says mercury makes your brain inflamed, which kills off your brain cells. Dad, do you have extra brain cells that you don’t need anymore? Wake up. I tell doctors all the time on stage, stop being nice. It’s not your job to be nice. Be kind. Kind means authenticity with compassion. You have to speak the truth of what you know. Don’t say, “well, they’re just resistant.” Well, then they’re going to die sooner than later of brain deterioration and Alzheimer’s. All this at the expense of the caregivers spending their time, money and their well-being trying to take care of this person they’ve loved for 50 years, who now is moving closer to being a vegetable. You (doctors) should say “wake up”. You shouldn’t put up with it.
Excuse me, but I had a patient, one of my staff who had worked with me for years. Her husband was just a wonderful, very kind, friendly man. He was a janitor in a grade school and the kids just loved him. All day, every day, walking down that hall they’d say, “Hi, Ray. Hi, Ray.” Kids, who sense energy so much better than we do, they just loved him. And I’d see Ray at our Christmas party or something and I’d say, “Ray, why don’t you come in and let me do a blood test for you to check about your cardiovascular system.” He’d say, “Oh, Doc, my doc says I’m fine. My cholesterol is not too bad. I’ve just got one medication, and it’s not too bad.” But he had creases in his ears. And those creases in the ears are strongly suggestive of coronary artery disease. Just Google “ear creases and cardiovascular disease”, you’ll see the pictures.
So I said, “I know Ray, but just let me do a test for you.” He said, “okay, Doc” but he never came in. Then one day he comes in. And he says, “Hey, Doc, can we do that test?” Of course I said, “Sure. Ray.” I drew the blood. And Ray left saying, “Thanks so much” I told him that I’ll have the results tomorrow. He replied, “Okay.” Ray drove home, he pulled over on the way home and died of a massive coronary on the freeway. So he probably came in because he felt something and didn’t know how to say it. So I don’t pull punches anymore. Not on my watch. If you’re my patient, excuse me, but I will be kind, but I won’t be nice. So stop being nice. And I say that to practitioners all the time, stop being nice.
Lindsey:
So the Total Tox Burden, is that a blood test?
Dr. Tom O’Bryan:
It’s a urine test.
Lindsey:
A urine test. Okay, so is that the best way to test for environmental toxins?
Dr. Tom O’Bryan:
Well, there are many good tests for environmental toxins. But this one from Vibrant is the most comprehensive I’ve seen and its sensitivity and specificity make it’s second to none. It’s right on the money.
Lindsey:
Okay. So are there gentle ways that people can slowly detoxify their bodies. Obviously removing the input of the toxins of course, but in terms of pulling it out, like a lifestyle change or supplements?
Dr. Tom O’Bryan:
Sure, of course, of course. First and most important thing is that “Mrs. Patient, your bloodstream is like a major interstate highway, two lanes in both directions, doing 70 miles an hour. And when it gets close to the cities, it opens up to four lanes and sometimes six lanes. But your bloodstream right now looks like it’s one lane, you’re backed up. Your bowel movements aren’t great, you’re backed up.” If you back your car up into a snowbank blocking the exhaust pipe, the exhaust comes into the car. So if you’re not having excellent elimination, you need to hydrate. And it’s a third of an ounce per pound of body weight. And if you’re sweating a lot because you’re doing saunas, or you exercise with a lot of sweat, it goes up to a half ounce of water per pound body weight. But you need to do that first before we do anything else. Don’t you dare take any nutrition to start detoxing until your highways are open so you can get this stuff out of you. And that’s the first step. And patients often notice that they just started feeling better right away because they didn’t know they were dehydrated. Look, you just pinch the back of your hand and let go, it should fall flat immediately. If it doesn’t, and you see a little ridge, you’re dehydrated. It’s not rocket science. It’s really easy to do. You’re smiling…
Lindsey:
I’m smiling because I have that and I drink water literally all day long. I mean, I’m taking sips of water constantly…
Dr. Tom O’Bryan:
Then you’ve got electrolyte imbalances, or some electrolyte is out of balance for you. The water is not being utilized properly. Your intracellular to extracellular water percentage is out of balance. I’m seeing you on the screen here, you have a little bit of a reddish tint to your face. That may be common for you or you may have been in the sun yesterday. But that’s inflammation for most people. You’re just inflamed. So the question is, why are you inflamed?
Lindsey:
I also put blush on, so it might be that!
Dr. Tom O’Bryan:
Okay, okay, that could be it. Also you have red glasses on and the frames could be reflecting that a little bit. Yes, yes. So you start with water, always start with water. Next is movement. The magic number is 9826 steps per day. If you do 9826 steps per day, the Journal of the American Medical Association tells us you reduce your risk of dementia by 51%. Just doing that, it doesn’t matter what you eat. I shouldn’t say that. They didn’t see any difference in the diets that people were eating, it was the movement. So 10,000 steps a day. And those two basics usually change a person’s metabolism and they start functioning better before you get to any detox of mold or heavy metals or anything else. And then you do your tests and you find out what do you specifically have to deal with?
Lindsey:
Okay, so say we’ve got those steps underway. Then are there supplements or foods that are great for gentle detox?
Dr. Tom O’Bryan:
Sure, there’s quite a few. There’s a whole category of the different phases of detoxification. There’s phase one and phase two, breaking down the chemicals that were exposed to in our lives today. That’s the first step for our livers to break down these chemicals and they break them down into an intermediate compound. But if you can’t break down those intermediate compounds and they accumulate, we used to call those pathological detoxifiers. People say, “Well, it’s a healing crisis missus.” No, it’s not. You just didn’t support them properly, but we didn’t know that back in the 1980s or 1990s. The science wasn’t out then in the way that it is now.
But yeah, there’s a whole world of things to do. Green leafy vegetables are always important, critically important. The cruciferous vegetables are critically important. I’m not so much into doing all these little things until you know what you’re dealing with. You don’t have time to waste anymore. Every autoimmune disease is going up four to 9% every year, and we’re still talking about well, “what can I do to help break down my toxins a little bit.” Dive in, dive in. Those that aren’t ready to dive in, they don’t want to learn about the toxicity in their home. House plants absorb 74% of the toxins in the air, if they’re not ready for all that I say, “all right, you know, I’m sorry, I can’t help everybody. Come back when you’re ready.” Right?
Lindsey:
Yeah. I’m just thinking like, you know, when you have an acute toxicity and you go see a regular doctor, they know what to do with that. Say you were acutely poisoned with lead or be it some other environmental substance…
Dr. Tom O’Bryan:
Well that’s to get them out of crisis, but they don’t get the toxins out of the body, right? They just get them out of crisis, right?
Lindsey:
And then they hide in the cells, and then you’ve got to pull them out of there. So are there particular protocols or companies whose products you particularly like for detoxification stuff?
Dr. Tom O’Bryan:
Yeah, it depends on your test results. I’m sorry, I can’t give you what you’re looking for. It depends on tests. For people who are interested in reversing, arresting or reversing the direction of their health, The Inflammation Equation has over 60 experts talking about, “What is this inflammation? Where does it come from? And what do you do about it?” I can’t summarize it in 10 minutes. It’s a nine day, one hour a day event. And every day we summarize it, and we say, “Can you believe when Dr. Bland said that?” Yes. Or, “Wow, well, that would mean if I did…, then that probably would help with this”, “Or when Professor Schoenfeld talked about 36%…Well, that that really reinforces how critically important it is to build a healthy, diverse microbiome.” Yes. Well, here’s how you build a healthy diverse microbiome. And that’s a 15 minute discussion on how to do that. Right. So there’s all of that available to read about.
Lindsey:
Yes. I do recognize that the longer I work in this field, the more complex things are and the more you realize the nuances of everything. So it’s not cut and dry that you can just quickly summarize these things.
Dr. Tom O’Bryan:
And everybody wants a quick fix answer. That’s what got you into the shape you’re in right now is going for the quick fix answer, and it doesn’t work.
Lindsey:
Yeah. So can you share a success story of how reducing toxic exposure has improved someone’s health?
Dr. Tom O’Bryan:
Oh, my goodness, yes. A 14 year old boy who had been to a number of celiac research centers, world famous ones, and was not getting better. He had a failure to thrive, he weighed 92 pounds and his bone age was three years less than his chronological age. His parents came to me and they were squeaky clean in how they were addressing celiac. And there was no error anywhere. They took their own silverware with them and pots and pans when they went on vacation so there was no contamination. They were doing everything right. And it turned out that he had a dysbiotic microbiome, meaning too many bad guys, not enough good guys in the microbiome, with severe intestinal permeability. And when you have a leaky gut, the exhaust of the bad bacteria get in really easily.
They’re called LPS, lipopolysaccharide. It is what causes sepsis, the number one killer of elders in hospitals. Accumulated LPS over a lifetime is what sepsis is and your immune system just can’t handle it anymore. But he had high levels of LPS. We identified that and we rebuilt the microbiome, detoxed him, got him doing gentle aerobic exercise to mobilize his highways in order to drain the toxins out of his system. And in a year and a half, he grew eight inches. He went from just under 90 pounds to 128 pounds in a year and a half. And now he’s five foot eight and a half, married, and very happy. This was a few years ago. It’s a classic example of when you have the best science but when you’re stuck looking at one thing so you don’t see the big picture, and then you can’t see where the obstacle is.
Lindsey:
So, wrapping up, can you just tell us about your recent book, and then where people can find you?
Dr. Tom O’Bryan:
Oh, thank you. Well, the Docuseries event will be coming up soon. It’s called The Inflammation Equation*. And when you go to the inflammationequation.com/parsons* and register, then a whole world opens up for you. And we just start educating you right away, even before the event begins. There’s a couple of books. I wrote The Autoimmune Fix*, which won a National Book Award, I’m proud of that. That book really explains where autoimmune disease comes from. And then I wrote the book, You Can Fix Your Brain*. And that was number one in seven categories on Amazon for brain function. And there’s 36 to “to dos” in there. So for those that want to know, “to dos”, what can I do on my own. You Can Fix Your Brain has 36 different “to dos.” For example, here’s three URLs for glass storage, go to mileskimball.com, amazon.com* and whatever the third one was, and you order glass storage containers*.
The secrets of success to all of this, the theme of our event is “progress not perfection.” And the secret to our event was that the subtitle of the book, it says it all, “there is just one hour a week to the best memory, productivity and sleep you’ve ever had.” And that’s the key to success. Everybody thinks we’re going for homeruns. And you’ll never win if you keep swinging for the fence, if you keep going for homeruns. People do this nutrition, this model, the next one, that one, etc. People say, “what about medium chain triglycerides, they help some people with Alzheimer’s” and then they quickly move on to something else. Stop chasing your tail. There’s no homerun when you have a degenerative disease. I always sign books the same way. I ask them their name and then write that name and I say, “base hits win the ballgame.” Keep going for the little things.
So just one hour a week. Tell your family every Tuesday night after dinner, “don’t bother me for an hour, I’m going to learn more how we can be healthy.” And then you go back to your podcast and listen to an interview again that they remember really liking or you go to my book and look at the three URLs for glass storage containers. Maybe you want three round ones and two square ones and one for the pie and you pay with your credit card. It took you an hour, but you’re done for the week. But never again will you poison your family with minute amounts of phthalates from plastic storage containers. Give the Tupperware to your husband to store nails in the garage. And then next week, you look at organic nail polish companies. And then next week you look at the list of houseplants. You go to my website, the dr.com/plants and get the handout from NASA on the house plants and you go buy a house plant. Then the next week you do one more thing and then next week you do one more thing, etc.
And in six months, you’ve completely changed your environment and completely changed the exposures you’re getting. And you see somebody at church and somebody says, “Wow, what happened to you? You look fabulous. What was it?” You reply, “Well, you know, I got rid of my plastic storage containers. I changed my nail polish. I got houseplants in every room. I found out that I did the blood tests and I’m sensitive to wheat and to dairy. So I lost 35 pounds when I went off wheat and dairy.” And your friend’s jaw drops because they’re overwhelmed by what you’ve just said. But you did it one hour a week. And that’s the secret to success, “progress, not perfection.” That’s the key. Progress, not perfection.
Lindsey:
That’s awesome. I think that’s a great point to wrap up on. Thank you so much for your time.
Dr. Tom O’Bryan:
Thank you so much. Pleasure to be with you.
If you are struggling with bloating, gas, burping, nausea, constipation, diarrhea, soft stool, acid reflux, IBS, IBD, SIBO, candida overgrowth, fatigue or migraines and want to get to the bottom of it, that’s what I help my clients with. You’re welcome to set up a free, 30-minute breakthrough session with me. We’ll talk about what you’ve been going through and I’ll tell you about my 3- and 5- appointment health coaching programs in which I recommend lab tests, educate you on what the results mean and the protocols used by doctors to fix the problems revealed. Or if you’re ready to jump in right away or can just afford one appointment at a time, you can set up an 1-hour consultation with me.

*Product and dispensary links are affiliate links for which I’ll receive a commission. Thanks for your support of the podcast by using these links. As an Amazon Associate, I earn from qualifying purchases.