Adapted from episode 150 of The Perfect Stool podcast and edited for readability with Shana Hussin, RDN and Lindsey Parsons, EdD.
Lindsey:
We talked a bit about what we were going to talk about, and one of the things that you like to focus on is insulin resistance and cortisol dysregulation, and that’s something that you’ve gone through yourself. So can you tell me about that?
Shana Hussin:
Yes, I know your story is similar and you’ve gone through the ringer with the gut stuff. When you’ve lived it yourself, I think it just becomes in your face and it’s easier to point people in the right direction. I’m a registered dietitian. I’ve been in the nutrition field for over 25 years, I taught the standard recommendations for a long time, and I was classically trained. Then, I discovered I had insulin resistance by following the standard nutrition guidelines and thinking I was doing everything that I should to remain as healthy as possible and feeding my family in the same way. Honestly, I didn’t know what insulin resistance was until about seven or eight years ago. Of course, I knew all about type two diabetes and pre-diabetes. there is very, very strong genetic diabetes, polycystic ovarian syndrome, heart disease, in my family, so I’ve always been really mindful about that and careful with my lifestyle. I noticed I was having a lot of cravings and food noise in my head. I would eat a meal, and I’d already be thinking about what I was going to be eating for the next meal, and even though my weight has never been a huge issue for me, I was doing a lot to maintain my weight. I was exercising a ton, I had three little kids, I’m like, “life just shouldn’t be this hard.”
And then, it’s kind of a long story, but my son got really sick, and I went into the deep thralls of alternative therapies, because the conventional system was not helpful for him and his healing. So, I went a lot of alternative routes, and I started to really dive deep into whole, natural nutrition and going away from the standard guidelines and was blown away by what I learned. Of course, intermittent fasting came on the scene, some therapeutic carb restriction therapies that I tried on myself, and I was blown away by the results that I saw. I actually wrote a book on fasting, and did that for a long time, and I mostly healed my insulin resistance, and again, I didn’t even know what that was. And what’s interesting about my story is that I always had normal blood sugars and normal cholesterol levels; my lipid panel looked great. Everything looked good on paper. I was in a healthy weight range, but once I learned about insulin resistance and how to test for it, I discovered that my fasting insulin was out of range on the high side, and at that time that I had my fasting insulin checked. I was already two years into this lifestyle of time restricted eating and therapeutic carb restriction, so I have no idea what my fasting insulin actually was when I was feeling all of the symptoms. I was able to reverse that, and I teach people how to reverse their insulin resistance.
But then, the second thing that you mentioned was that I also teach mostly women, because women are who really struggle with a lot of cortisol issues. Funny enough, when I was doing all of the things that I teach, and intermittent fasting in a way that I was I also kind of exacerbating my cortisol issues that were already there. For the longest time, I thought cortisol was all about managing your nutrition and managing your stress, which play a strong role. But that wasn’t the biggest piece of the puzzle. Again, I went down this deep dive into how to actually fix cortisol issues, because I just see it rampant in the people that I work with, women my age, who are in perimenopause and menopause. But even that, I had cortisol issues since college, I would say they started, and I just didn’t know how to fix them. So, long story short, I discovered how to fix my cortisol issues. Once I did that, once I brought my cortisol levels back into balance, I fully recovered from insulin resistance, because I still had a little bit of insulin resistance hanging on until I balanced that hormone. So that’s how I got into specializing in those types of issues.
Lindsey:
Got it. So you were mentioning your fasting insulin being elevated, and I assume you meant according to standard reference ranges. But, I have heard that for fasting insulin, below six is an optimal reference range. Is that something you use as well?
Shana Hussin:
I do. So when I first tested mine, and I was two years into this lifestyle, mine was 10.7, so if I had gotten that result in the conventional system, they would say fabulous, “that looks great.” I knew that it was at least slightly elevated. Again, I’m willing to bet it was probably in the 20s prior to that, when I first started working on reversing it. In the conventional system, most lab standards are up to 24.9 as being normal, which really high. So yeah, as you mentioned, I like to see that number between 2 and 6. When I first had mine tested, it was 10.7 and then I had it tested two years later, and it was 7.5 and I was still like, “what the heck? This is like four or five years later!” Not that it was extremely elevated by any means, but it was still outside that normal range. Once I balanced my cortisol and brought that last piece of the puzzle in, which was working on my nervous system and my lighting environment, then my level went to 2.2 and that was just this past summer, so just a couple of months ago, so I was really happy to see that.
Lindsey:
Awesome. So I’m curious, because I have a client in this situation. So what does it mean if you have somebody who’s not diabetic, but they have a lower than 2 fasting insulin?
Shana Hussin:
Yeah, that can happen. You don’t want to have no insulin response whatsoever, but so you do want to have some. Under 2, in my experience, and this isn’t always true, but sometimes they can have higher than normal blood sugars because they’re just not secreting enough insulin to draw the blood sugar into the cell. Sometimes, as with type one diabetics, they don’t produce any insulin.
Lindsey:
Right. It’s gone so far into insulin resistance, they don’t have the insulin coming.
Shana Hussin:
Exactly. Yeah, that’s an interesting scenario. Either their pancreas is needing some help, or I’d be willing to bet their blood sugars are probably a little bit higher.
Lindsey:
Yeah. So I came into the functional medicine field when the term “adrenal fatigue” was coming under criticism, and I know most practitioners now call it an HPA Axis dysfunction, but the same type of diagnoses and treatments are administered, whether it was called adrenal fatigue or HPA Axis dysfunction. So, if someone has low DHEA and lower high cortisol, no matter what it’s called, the people I trained under, they’re giving pregnenalone, they’re giving DHEA. So I’m curious what your take is on all this and the terminology and how you deal with it.
Shana Hussin:
Yeah, and HPA axis dysfunction is definitely more accurate than adrenal fatigue, and in the conventional system, adrenal fatigue, adrenal dysfunction, adrenal exhaustion, all of those terms are pretty much dismissed by conventional doctors most of the time, unless there’s actually something wrong with the adrenal gland, in which case, their only solution is typically medication. But as you mentioned, we know now, hopefully more and more people will be starting to know that it’s more of an HPA axis dysfunction. Cortisol is produced by the adrenal gland, but it’s produced in response to the signaling that it’s getting through the eyes and the light environment. So the light that’s coming into the eyes – eyes are basically an extension of our brain that is signaling to the hypothalamus what to do and what time of day it is, and basically telling the body what to do, when to secrete hormones, when to make neurotransmitters, when the organs should be doing what they’re doing. The hypothalamus then tells the pituitary glands to tell the adrenal glands to then make cortisol.
And so we blame the adrenal gland and say it’s adrenal fatigue – the adrenal gland is just tired, which you know in some circumstances might be true on some level, but it’s mainly just the communication that has been broken. The body is so confused by all of these different signals that it’s getting that we were not meant to take in through our eyes. That signaling is broken. And so the adrenal glands just don’t know what to do. They don’t know when to secrete cortisol. They’re secreting it at times of the day that it’s not normally secreted, or they’re not secreting it at certain times of the day when it should be secreting it. And so that’s where we do go back to that HPA axis dysfunction and being much more accurate. And in functional medicine, they’re definitely starting to come around. But I know with functional medicine too, a lot of times people would go in with cortisol dysregulation or imbalance. And the response was, “well, let’s give you adaptogens, or let’s give you ashwagandha.” And those things can certainly help. I’m not disregarding those, but it’s still not fixing the messaging along the HPA axis.
Lindsey:
It sounds like you’re using light. So is this about following a circadian rhythm, getting light in the morning, low lights at night, kind of thing?
Shana Hussin:
Yeah, that’s the main therapy, and the main thing that I have my students work on when they come to me. First, we’re looking at cortisol testing and looking at what their pattern is during the day, and we can talk a little bit more about that, but what their pattern is showing is how we’re going to set up their therapy, but it is primarily light focused. So I know for me, I got to the point of adrenal exhaustion. So the testing that I like my students to do is called a four-point cortisol saliva test. And maybe you’ve mentioned this on the podcast before, and the one that I have sent, I have a home kit sent to them that also includes the hormone DHEA, because usually that’s really low when the adrenal glands are not working correctly. It’s a salivary test; you spit into test tubes at four times throughout the day.
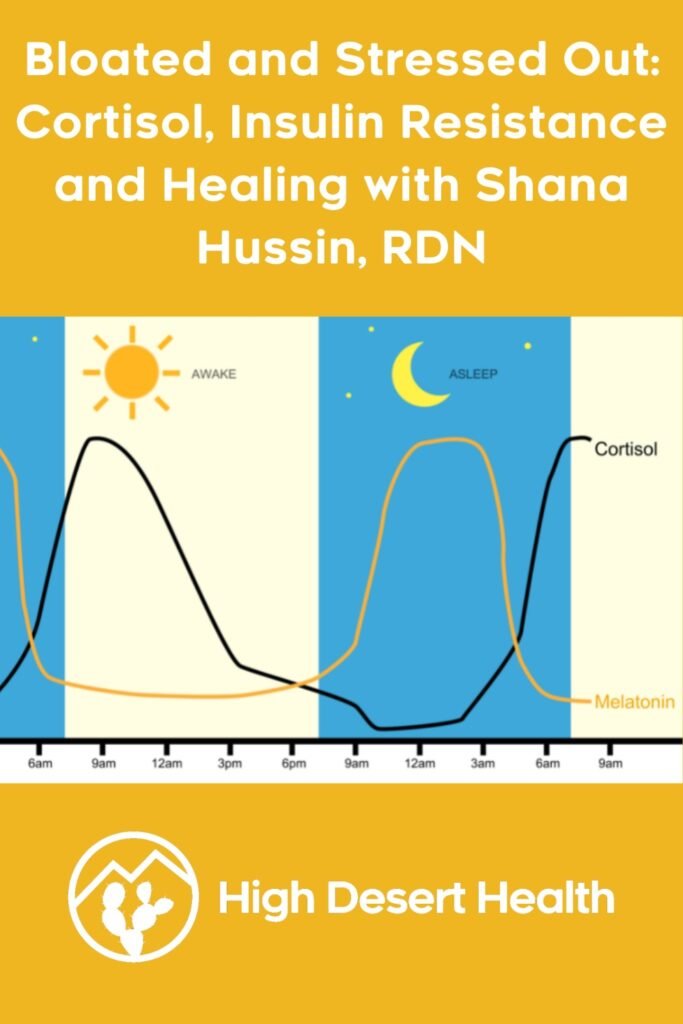
But why that’s helpful is that we should have a natural cortisol spike in the morning, when we’re getting up, it’s our system saying, hey, let’s get up and go. And then it should kind of peak midday and then start to fall, and it should be low by late afternoon to evening. A lot of times I see either a flattened cortisol pattern like I had, where it’s just kind of low levels of cortisol all day long, and that’s usually when this has been going on for a really long time. Things are just very chaotic and dysregulated by that time, the signals have been off for a really long time, or a lot of times, I’m seeing an inverse pattern where people are having high cortisol levels at night, and that sets us up for very disturbed sleep and not healing and feeling like absolute crap all the time, because you’re not getting restorative sleep. It can lead to weight gain, and so you have these levels of cortisol going high at night, in the afternoon and in the evening, when they’re supposed to be falling, and that prevents us from going to sleep and staying asleep. People who are feeling wired but tired at night because they just can’t seem to fall asleep, they’re wiped but they can’t fall asleep. What happens is the cortisol goes high at night when it’s supposed to go low, and the inverse hormone is melatonin, and melatonin is our fall asleep, stay asleep, repair hormone, and that should peak at night, but instead, cortisol is high, and so we can’t fall asleep, stay asleep. We have very dysregulated sleeping.
And then come morning, when our cortisol levels are supposed to be going high again, they’re very low, because this whole inverse relationship is off with melatonin and cortisol. So that is where a lot of these issues are coming from. But like I said, I like to test my students first to see what their pattern is. My therapies or the suggestions that I make are very, very similar, but knowing what we’re starting from and where we’re starting from with cortisol patterns is really helpful. So then you’re just doing that saliva test at four times throughout the day to see what your pattern is, if that cortisol level is rising falling as it should be. It’s a really easy test to do, and we can track that over time. I know I struggled with this for decades, and like I said, I got to the point of adrenal exhaustion. Once I learned how to properly incorporate and change my lighting environment and work on my nervous system, I was able to recover my pattern within a couple of months. So you know what’s causing it and how to correct it. You can do so pretty quickly. You can kind of go by symptoms, but I like to test and then test every three months or so to make sure that that cortisol is still well in balance.
Lindsey:
Yeah. And so how can you correct that dysfunction? Or how did you do it for yourself?
Shana Hussin:
Yeah. So as I mentioned, mine was just low all day long. It’s weird, because a lot of times when people are to the adrenal exhaustion stage that I was at, they’re so tired, not wanting to get out of bed. And a lot of times they’re misdiagnosed with depression with really low levels of cortisol, or they’re diagnosed with anxiety when cortisol is spiking at the wrong time. It’s really kind of sad because had I gone to a conventional medicine practitioner, I probably would have been offered an antidepressant, or if I had high cortisol night, an anti-anxiety medication.
But what I did is I learned how sunlight and our lighting environment really are the triggers for cortisol, the main triggers. There are other things, I’m not going to say it’s just light, but that’s the primary one. When sunrise comes into our environment in the morning, at daybreak (daybreak and sunrise are different) – daybreak is when the light is starting to come into the environment. Sunrise is when the sun is actually coming onto the horizon. At daybreak, there’s a lot of red light. And if you go outside, it’s like that warm glow. It’s kind of reddish looking. So a lot of red light there. Sunrise is where blue light comes into the environment, and it’s in the same amounts as red light. When blue light comes under the horizon, and our eyes can take that in, it’s the blue light that is picked up by the eyes that tells our body to produce cortisol. What happens is, people aren’t going outside much, right? The average American spends seven minutes a day outside, which is astounding. We did not live like this a couple hundred years ago. Our environment has changed so drastically, and our genetics have not had time, they really haven’t changed at all. They haven’t had time to catch up with all of this lighting change.
And so, going back to sunrise, if you can go and watch the sunrise, you will tell your body to produce cortisol. Mine was really low, so all I did was go outside every single morning at sunrise. I miss some in the summer because I live in Wisconsin, and sometimes the sun is coming up at like five o’clock in the morning, but as much as I could, I went outside to see the sunrise, and that triggered cortisol production. And the cool thing about the sunrise and the natural light in the morning is that it’s going to act as if your levels are too high, it’s going to bring them down lower. If they’re too low, like mine are, it’s going to stimulate that cortisol to be higher. So that was a huge part, just getting outside, going out to the sunrise. I’m not saying you have to sit out there for an hour. I set a timer for three minutes. If I can sit out there for longer than that I do; otherwise, I go out for three minutes just to get that signaling into my eyes.
As we go throughout the day, our lighting is always changing outside, the spectrum is always changing. At midday, we have very high levels of blue light, not as much red light. And then we get into sunset, and there’s a lot more red light than blue light. And then after nightfall, there’s no blue light in our environment, and that’s important to take into consideration, because remember, blue light stimulates cortisol after nightfall. As humans, we’re not supposed to be getting those signals of blue light into our eyes anymore. We’re supposed to be winding down and going to sleep. But what has happened in our environment is then we stare at TVs, we stare at phones, movies, Netflix, computers, we have to do homework, iPads, whatever it is, and all those things are very, very high in blue light. So this is where that inverse pattern is coming into play as people who after nightfall, after dinner, after it gets dark, they’re watching TV all night, or they’re working all night.
Sometimes we have to work – night workers, hospital workers, who are under these awful, awful fluorescent lights throwing all this blue light your body is perceiving that at all times. And so it gets really confused. It’s nine o’clock at night, and your body’s like, “Wait, I thought the sun went down, but all this blue light’s coming in. It must be midday. Oh, I better push my cortisol up. I better give Shanna some more cortisol, because it’s midday. She needs more energy.” Cortisol levels rise, and it makes it so hard to go to sleep. And the thing about cortisol, too, and why I wasn’t fully recovering from insulin resistance, is it also increases blood sugar, it increases insulin. It’s interesting. There are so many studies, even if you are not eating or you’re not hungry, you start to watch TV, you put a phone in your face, and the cortisol is stimulated. All of a sudden, you’re having cravings. You’re having “I want some ice cream,” whatever it is, the cortisol goes up, the blood sugar goes up, insulin goes up, and it’s really tough to reverse that insulin resistance fully. That’s the main thing I did to fix mine, just go out at sunrise, and I’d go out for light breaks throughout the day, and I don’t wear contacts or glasses, but you want to do this with naked eyes, if at all possible.
Lindsey:
Right. And not through windows, right?
Shana Hussin:
Not through windows. You can open the window and look through screen. That’s fine. If you’re driving, you can crack a window, but almost all UV light, and most red light is filtered by windows. Unfortunately, yeah, looking through the windows isn’t the same, no contacts, no glasses. I did a lot of light breaks. I did a lot of other things for my nervous system, like grounding and being in nature. Another thing that I did that I had no idea was exacerbating my cortisol issues was I stopped wearing sunglasses. And I know that that sounds really wonky for a lot of people. I live in Wisconsin, if it’s snowy, if I’m driving and there’s glare off the snow, or if I’m boating and there’s glare off the water, then of course, I wear sunglasses. But for the most part, I stopped wearing sunglasses because that’s confusing to the body too, because it’s filtering all the light signals.
Lindsey:
Yeah, and what color are your eyes? I’ve got to ask.
Shana Hussin:
They’re green.
Lindsey:
Mine are too, and mine are so sensitive to light I cannot stand to be outside without a hat and sunglasses. I live in Arizona, so.
Shana Hussin:
Mine used to be that way, Lindsey. It’s interesting because I had very high light sensitivity, and that’s another sign of adrenal fatigue and adrenal dysfunction. And I was a lifeguard and growing up, and I’m like, “How am I going to stop wearing sunglasses? This is crazy.” But I just did it little by little, I started with a hat, and now I can go out. It’s really crazy. I don’t have to wear sunglasses anymore.
Lindsey:
You aren’t squinting the whole time?
Shana Hussin:
Nope. In the summer, at high noon, I’ll put a hat on, or I like to work outside, and if I’m able to, I’ll sit in the shade. But that light sensitivity goes away with time, and it’s just because you’re so accustomed to being indoors and to having sunglasses on. All of those things, within a couple of months, I tested my cortisol pattern again, and it was normal. And I’ve never been a night hawk, so nighttime wasn’t a huge factor for me. But the other thing that’s so important is blocking the blue light after the sun goes down.
Lindsey:
Right. I also just heard, I was listening to the Huberman Lab podcast, and he was saying that there was a study that they were questioning the whole blue light hypothesis, and that maybe it’s not even the blue light, but maybe it’s actually the devices themselves and the amount of stimulation that they’re giving you that’s raising your cortisol, not the light coming off of them. I’m sure the jury’s still out on that question. It’s probably just one study.
Shana Hussin:
I would say both for sure.
Lindsey:
Without question, the stimulation of scrolling through social media and things like that.
Shana Hussin:
Oh, for sure. I’ve been wearing blue light blocking glasses for like a year. And I will say if I’m watching a stimulating show, even with my blue light blocking glasses on, I have an Ouro ring that tracks my stress response. My husband and I have been watching Yellowstone, and when I watched that right before bed, I watched my stress response climb. I’m like, “Okay, I’ve got to do my glasses and I’ve got to do my wind down routine.”
Lindsey:
I know, I don’t like watching scary things and that sort of thing. My son got us watching this “Killing Eve”. And I’m like, “This is brutal. I don’t like this. I don’t want to watch this kind of stuff.” Anyway, I’m wondering why cortisol seems to get imbalanced, in particular with women in perimenopause/menopause. Why is that a thing?
Shana Hussin:
I don’t have the exact answer, but I draw my conclusions. I just turned 49 so I’m in perimenopause, and I work with a lot of ladies in perimenopause, but you get more insulin resistant when you go through perimenopause just because of all of the hormonal changes. So we can’t do the same things as we used to do. We can’t eat the same way, our stress response….
Lindsey:
Or drink the same way. Can’t do anything the same way after you lose that estrogen.
Shana Hussin:
Yeah, your skin changes, your hair changes. You’re not as resilient. So I don’t know what comes first, the chicken or the egg with cortisol or insulin resistance. I honestly think it’s a combination of all of the above. You know, you’re probably the same type of person I am: type A. I raise three kids; I run a business. I want my kids to eat well. We just have busy woman syndrome. And I think by the time we’re in our 40s, 50s, our hormones are declining. We’re not as resilient as we were before. We’re more apt to store body fat because of the estrogen levels falling. We don’t sleep as well. We’re not as like, “Oh, get up and go and conquer the world.” Everything comes to a head, and we’re just at the time in our lives where my kids are older, two are in college, and one is in high school, but I lost both my parents last year. We’re just sandwiched into raising our kids and taking care of our parents and going through all these hormonal changes that is just a really hard time for women, and that mom transition too, where I was so busy with my kids for so long,. . .
Lindsey:
I just have one at home. And he drives too!
Shana Hussin:
And now, what am I going to do all the time?
Lindsey:
Have fun?
Shana Hussin:
Like I said, women want to eat and drink and do the same lifestyles they did in their 20s, but now we have all of those changes coming at us, and we start to show some symptoms as a result.
Lindsey:
It’s shocking how your health plummets when you start to lose that estrogen. I’m on hormone replacement therapy, and even still, my cholesterol has gone up, blood sugar’s gone up. Admittedly, my last blood tests were after my honeymoon, because I got remarried, and I had been drinking every day because I was in France, and that’s what you do.
Shana Hussin:
Well, their alcohol is probably completely different. You know, everything’s different there.
Lindsey:
I mean, whatever the quality of the alcohol, my liver enzymes were certainly above optimal by the end of that. I’ve been waiting to correct this all and retest and hopefully get better numbers, but still, just going into menopause shot everything for me, really, and I’ve been reading about that and what the alternatives are to even just your basic HRT. But looks like the alternatives are not great. If you really want to replace your hormones back to pre-menopause levels, which is what the authors of book I’m reading are proposing, you actually have to have a period, potentially even get injections of estrogen. I’m using a patch and progesterone pills. So it’s not crazy.
Shana Hussin:
That’s the one benefit of going through menopause, right?
Lindsey:
Exactly. I’m like, “I don’t know it’s a tough trade off, but I still get the hot flashes even when on HRT.”
Shana Hussin:
Right, it’s like, “I want my hormones, but I don’t want that anymore, exactly.”
Lindsey:
So when somebody does have that spike right before bed in cortisol, other than keeping out the blue light and dimming lights, is there anything else that can be done about that?
Shana Hussin:
Yeah, so the blue light is the main thing. And when I start to work with people with cortisol dysregulation and insulin resistance too, the first thing that we work on is our nighttime routine, because it’s hard to fix the morning routine when you’re not sleeping well. So getting that under wraps, starting with the blue light blocking, and I will say there are more and more blue light blocking glasses coming out. And you can get them on Amazon; you can get them wherever.
Lindsey:
Or if you wear prescriptions, you can get them built in, like I’ve got.
Shana Hussin:
Yeah, but unless you’re wearing the orange toned at night, the clear ones aren’t going to block the blue light. They’re going to help with eye strain with your computer if they’re clear, but you want the orange tone or the red tone. I don’t wear red tone. I don’t need those. But the orange tone, I’ve switched out my light bulbs in my living room and my bedroom so that there’s almost no blue light. They’re 99% no blue light.
Lindsey:
Okay, so what kind of light bulbs does one get?
Shana Hussin:
They’re called Hooga, H, O, O, G, A, is the company that I order from, Incandescent lights will also have virtually no blue light. They were almost banned for a long time, but there’s now an executive order signed that incandescent lights can be sold again, and I could always get them in Wisconsin, but there were certain states, I know California for sure, you couldn’t get incandescent light. So the LED lights, the really bright, fluorescent lights, are the ones that are problematic. And then, of course, just having some kind of wind down routine. I try not to look at my phone or screens at least an hour before I want to sleep. I’m reading or I’m journaling, I know that’s not for everybody, but that really, really helps.
Some other things that can help if you absolutely are having trouble sleeping, magnesium. We mentioned progesterone. You might need to look into that, but people are amazed at what blocking the blue light does with sleep quality. So we start there and work on the nighttime routine, and then the daytime and morning routine become a lot less challenging because you’re getting that melatonin peaking at the correct times. I tell my clients I work with, if you can be asleep by 10 o’clock, that is where I want you eventually, because all of these repair systems and the melatonin production peaking, melatonin peaks about four hours after darkness and after you’re sleeping. If you’re falling asleep around 10 o’clock, it’s peaking around 2 a.m., which is when it should be peaking, and then it’s starting to fall by the time you want to wake up.
People who don’t go to sleep until midnight, or they have this blue light in their eyes, they’re not letting melatonin take over until 12, one o’clock in the morning, while it’s peaking, then at 4 or 5 a.m. That’s why you don’t want to get up, because your melatonin is high, your cortisol is low. And there’s people who are like, “I’m a night person, I’m a morning person,” and there’s definitely something to that, but a lot of times it’s just this dysregulated light environment, and then the morning routine becomes a lot easier. You’re able to get up and watch the sunrise and take in light breaks throughout the day, and that’s kind of where we start. But the melatonin production is just as important as the cortisol, because if you’re not healing and repairing and getting restorative sleep, it’s going to be very hard to recover from any disease.
Lindsey:
What about other patterns I’ll often see, like on the Adrenocortex or the ZRT four-spit cortisol test/adrenal test is that someone’s cortisol is particularly higher in that sort of 5 to 7 p.m. range. I think that’s probably a natural rhythm of life. Just because that’s when we’re doing all the stuff. We’re finishing work, we’re picking up kids, we’re making dinner, we’re running errands. Those are naturally high cortisol things. So is that something that needs addressing, or is that sort of a natural period of higher stress?
Shana Hussin:
Yeah, I mean, it should be a little bit higher, that kind of mid to late afternoon, but it should be falling. I’ve seen that pattern for sure, where it’s out of range at that third time that they’re doing the spit test. But what we work on then is getting wound. I think that this is probably me, like, 10 years ago, where I’m taking my kids everywhere and you know, your workday kind of ends, but then it’s just beginning of the whole nighttime routine. So yeah, I do see that pattern, and a lot of times it has a bit to do with the blue light stimulation again. But it’s important to note, if you are working on getting cortisol back into balance, like I said, I primarily did all the lighting things, but I also had to work on my nervous system, like I was just in this perpetual fight or flight all the time. And some of that was everything that happened with my parents, but it was just that, like I mentioned, that busy woman syndrome too.
Or I just tell myself, you’ve got to slow down, you don’t have to be achieve, achieve, achieve all the time. And so I started things like journaling, Bible reading, just quiet time that I had never incorporated in my day before. And there’s a couple of other things that I teach in my course to really work on the nervous system. It sounds kind of crazy, but doing a couple of cold face plunges in the morning just takes you out of that fight or flight. You can feel it immediately. So there might be people who have that pattern as well, and as long as you can get it lowered by the time you go to bed, it’s not going to be as disruptive as a real high cortisol at bedtime.
Lindsey:
So what is leptin, and what does it have to do with blood sugar and cortisol?
Shana Hussin:
Leptin is another hormone. It was only discovered in 1994- I mean, it’s always been there, obviously, but we didn’t really discover it until 1994 and not a lot of people know about leptin or what it does, but it’s actually produced in the fat cells, and its primary job is to tell the body what’s the energy status on my body. This becomes very, very important, because leptin, telling the brain what the energy status is of the body will give it signals for hunger, satiety, how much to eat the next day. We can back off. We’re not as hungry the next day. But leptin, like I said, is produced in the fat cells, and it can become dysregulated. I see it mostly become dysregulated in women who have tried their entire life to lose weight, and they’ve kind of been in this caloric deficit, gain the weight back. Caloric deficit, gain the weight back. The perpetual dieter almost always has dysregulated leptin.
And the other thing that really screws up leptin is snacking and eating, and this perpetual I’m just going to eat and graze like the grazers. And so what leptin does is it docks to the brain, the hypothalamus, usually around midnight or so, and it downloads. It gives the body a download, like, “Shana has this many extra calories stored as body fat,” or “Shana really has no energy stored.” And what that does is it tells the body how much to eat the next day. So if there’s leptin resistance where your leptin is too high, this happens usually when we have too much body fat, when we’re in that perpetual snacking, grazing mentality, the fat cells are just producing too much leptin.
This is a problem because it’s just a miscommunication to the brain and then the perpetual dieters, restrictors. Those who’ve been doing a lot of fasting or a lot of caloric restriction, they can’t seem to lose weight a lot of times, they have really low levels of leptin, and that can become problematic too, because then you might have extra body fat. Your brain is being told you don’t have energy stores and to eat a lot the next day. When we’re leptin resistant, we’re almost always insulin resistant too. The thing that people should know about leptin is that it’s docking to the hypothalamus around midnight, but the receptor, the leptin receptor, competes with insulin, and so if you have higher than normal levels of insulin, it’s really hard for leptin to dock at the hypothalamus where it should, and your body’s not getting that communication either. So if you’re insulin resistant, a lot of times, we’re also leptin resistant, and we’re just kind of a hormonal mess.
And the other thing that’s really important to note about leptin is it primarily docks overnight, and so what I’m getting at is you don’t want to be eating at night, and you don’t want to be insulin resistant. You’re eating at night, and you have high blood sugar, high insulin, your leptin is not going to dock correctly. So that’s really important. So that’s a whole another thing that I work on with my insulin resistance folks is to stop snacking and stop eating at night, so your insulin can come down and your leptin can start to dock to your brain. Leptin will also download during the day about every four hours, and that’s why when we’re eating correctly and we’re managing our blood sugar and our blood sugar levels are healthy, we should be able to go 4, 5, even 6 hours without eating if our leptin is signaling correctly, and you won’t get a leptin download until about four hours after you’ve last eaten. So if you’re just in this perpetual snacking mode, your leptin is probably very dysregulated, and you’re going to have a really tough time losing weight, and just metabolically, you’ll struggle.
Lindsey:
So are you measuring leptin on your clients? And if so, what’s an optimal level?
Shana Hussin:
Yeah, I wish. You can. You can ask your doctor for leptin, but chances are they might….
Lindsey:
Chances are they’ll say no.
Shana Hussin:
If they’re more progressive, they might. I also work with ZRT. You mentioned ZRT earlier. This is the lab that I order all my own kits from too, they don’t have leptin right now. I’m hoping that in the near future they will. You can order it on Own Your Labs. Some of those lab websites where you can order up what you want and go to, usually it’s Quest or Lab Corp that will test it. I like to see a level like 2 to 9 somewhere in there, but unless you get it checked, you don’t really know. But it is important to look at your levels. Way over 9, it’s going to be a little bit different approach than if you have really low levels. And usually, like I said, my low leptin people that I’m seeing are those who are type A, over restricting in a caloric deficit. Maybe been over fasting for a long time, important to have that in balance too.
Lindsey:
Yeah. And so the solution to that is just eating normally, not restricting your calories?
Shana Hussin:
Yeah, yeah. So how I go about fixing that, I used to do a lot of intermittent fasting throughout the morning. So we fix insulin resistance at the same time. The very first thing I have my people stop doing if they’re insulin resistant is snacking, and we just go to eating three square meals a day to begin with, protein centered, having some natural fat, having strategic produce in there, getting that under wraps first, along with working with the whole lighting thing at night so that you’re not hungry and wanting to snack, and cortisol going crazy. It’s a lot. It’s a lot. People are like, “Oh my gosh, there’s so much to do.” But really, once you understand your hormones and the environment that is giving your hormone signals, you can start to fix it. The main thing is three square meals, allowing eventually to go at least four hours in between meals so you can get that leptin signaling in between meals, stopping the night eating for sure. And then we do go therapeutic carb restriction, at least for a while. And I’m not saying everybody’s got to go ketogenic or anything, but that does help to bring insulin levels down.
Lindsey:
When you say carb restriction, how much? Obviously keto, you’re eating maybe 20 grams of carbs a day or something.
Shana Hussin:
Yeah. I actually have a carb quiz on my website to help people with this. Everybody’s different. It’s why I like to work with people individually. But generally I’m recommending 25 to 100 grams of carbohydrate a day, less restrictive around the 100 grams, and then somebody who’s really insulin resistant, like they’re requiring insulin, they’re on all kinds of diabetes medications, that would be more of the let’s eventually get you to around 25 grams of carbs, 50 maybe, until your body is utilizing carbohydrates a little bit better. Because usually you know you’re at that point, you’re very insulin resistant. You’re not utilizing carbohydrates well at all. That’s not forever, but for a time, bring it down. I have people carb flex in there and bring carbohydrates up, maybe one day a week, a couple times a month. I don’t like the perpetual, “let’s eat low carb, 25 grams of carbohydrate every single day for the rest of our lives.” I don’t think that’s healthy.
Lindsey:
Yeah. And so they’re not replacing those calories necessarily with fat, right? Or is it adding more protein, typically, that you’re looking at?
Shana Hussin:
Yeah, I have people build their meals around protein because it’s very satiating. It’s what we primarily build our body with. So, in general, I’m having women eat around 100 grams of protein throughout the day. When you meet that, you start to have those hunger and satiety mechanisms come back. I definitely have seen in my practice, people overdo fat and go way too high on fat, and then they’re struggling to lose weight, because even though they’re burning ketones and they’re burning fat for fuel, they’re burning fat that they’re eating, they’re not burning fat from their body. And so that’s where the time restricted eating comes into play, and the whole leptin resistance thing, because if your leptin signaling is healthy, your body will say, “oh gosh, I have 50 pounds of extra body fat here. I don’t need to eat a whole lot today,” and it will downregulate your appetite and all of it. It’s just all interplays so beautifully when it all works correctly.
Lindsey:
Before we run out of time. I want to bring it back to the topic of my podcast, which is gut health. So how does all this relate to your gut health?
Shana Hussin:
Yeah, it’s fascinating. With cortisol, what I found was really interesting, and what I was struggling with my own gut health was a lot of bloating and a lot of food that wasn’t being digested well, and this is because I was in overdrive. I was in that fight or flight, and my body was so stressed out that instead of taking all the energy for proper food digestion, it just couldn’t digest.
Lindsey:
You were not in rest and digest.
Shana Hussin:
Exactly. I was not in rest and digest. I was in fight or flight, and so almost every meal I would be bloated. I had more food sensitivities than I do now. That’s just one little thing. What really helped me, and this is in my adrenal recovery course, is I took betaine HCl and digestive enzymes for a time with every meal, and I still do that on a lot of days with bigger meals, and that helped to start to digest my food properly and stop that bloating. And another thing with digestion, with insulin resistance and eating too often, is we’re just not giving our digestive systems a break ever. And so that’s why, again, going to two or three meals, and I think it’s perfectly fine for some people to eat just one meal a day. Some of the time when they have a lot of weight to lose, but giving your body some rest and digest and rest and repair is so helpful for the digestive system. And if people do want to intermittent fast and inside my courses, we do have a more of a circadian approach, where we’re fasting late afternoon into evening, to really support the autophagy process during sleep and give that digestive system a nice, long break.
Lindsey:
As opposed to the skipping breakfast model, right?
Shana Hussin:
Yeah.
Lindsey:
The problem is nobody wants to skip dinner. Everybody likes dinner, and they want to eat it with their friends or family or whatever. And so it’s got to be challenging but makes way more sense metabolically.
Shana Hussin:
It is more socially challenging for sure. It has a lot more benefits. People are doing the habitual, and I did that for like, 5 or 6 years, and that just dysregulated my cortisol even worse . . .
Lindsey:
Yeah, I’ve heard it’s not good for women, the whole skipping breakfast thing, and maybe not good for anybody. I’ve interviewed the ProLon Fasting Mimicking Diet* folks, Joseph Antoun, he was saying that, in fact, if anything, skipping lunch, if you don’t want to skip dinner, skipping lunch would be a better choice than skipping breakfast.
Shana Hussin:
Yeah, if you can be done eating by 3, 4, even 5 o’clock, that gives you a nice long break. I skipped breakfast way too many years, and it took a toll on me, and I started to have high blood sugars throughout the morning because my cortisol was out of balance.
Lindsey:
Yeah. There’s no way I could skip dinner, though, I have to say, because I’m just somebody who’s got a super-fast metabolism. If I skipped dinner, I wouldn’t sleep a wink, because I’d be sitting there with hunger pangs all night. So one last question, which is how cortisol, melatonin and leptin interact.
Shana Hussin:
Yeah, I like to call these three hormones the master circadian hormones, for all of the reasons that we already discussed. So if cortisol levels are off and melatonin levels are off, your body’s just in chaos and not signaling correctly. But those three hormones are above a lot of the downstream hormones. So if your cortisol and melatonin are off, there’s a hierarchy of hormones, and if you’re filtering all your energy into that cortisol, you’re not going to filter the energy into making sex hormones. It’s just so intricate, and once one hormone gets off, especially if it’s cortisol, melatonin or leptin, all of the downstream hormones, I don’t want to call them more important, but reproductive hormones can be out of balance and not affect us as much. They’re not life or death, right? It’s just “okay well, our fertility is going to not function correctly, but if we don’t have cortisol, we’re in big trouble. If we don’t have some of the other master hormones, we’re in big trouble.” When melatonin, cortisol, leptin are off, people have a lot of weight issues, a lot of chronic illness.
And the nice thing is that fixing them, we do it all in the same way. We get a strong circadian rhythm, we dial in our nutrition, we fix our lighting environment, all the foundational things. And really, when you think about it, just going back to being human, how humans are meant, like we’re not meant to be – my whole business is online, so we sit inside, under artificial light, staring at computers. That’s so much different. And then we eat by our desk, and we don’t socialize. I’m not saying everybody does this, but when you think about humans, even 200 years ago, as to now, things have evolved and changed so quickly that we just haven’t caught up. A lot of our bodies are internally in chaos, and we can’t understand what’s going on. But when we stop and think about how different our lifestyle is, it’s no wonder that we’re all sick and struggling.
Lindsey:
Yeah, no, I think you really have hit on it too as it relates to gut health, how you start with these dysregulated patterns and then it has all these bad downstream effects. A lot of people that I see have gut health issues that ultimately seem to have stemmed from stress, and often a particularly stressful period in their life where, clearly, their cortisol starts to get dysregulated, their blood sugar gets dysregulated, then they lose their immune resilience. Really, I mean, their immune system gets weakened, and I can see it in their Secretory IgA levels on the stool tests that their immune systems are no longer functioning, but stomach acid levels have gone down. So there’s no protection. So then all of a sudden, these pathogenic bugs start to take over, and then you start getting all these gut symptoms, and it just snowballs from there. So yeah, it really does start with these patterns that come under stress and cortisol.
Shana Hussin:
I like to tell people we need to fix the terrain. There is a reason why you are having all these imbalances, and the terrain is off, a lot of it has to do with not getting out into the sunlight, not getting proper messaging, eating crap that doesn’t belong in your body, and not sleeping.
Lindsey:
Yeah. So tell me where people can find you. And you do courses, yes?
Shana Hussin:
Yes. If you go to ShanaHussinwellness.com, all my courses are housed there. I have lots of freebies. I have a free eBook on cortisol dysregulation. I have a cortisol minicourse as well, if you want to learn the basics of how it gets dysregulated and how to start to fix it. And then I have a podcast called Optimal Metabolism.
If you’re dealing with gut health issues of any type (diarrhea, constipation, bloating, SIBO, IMO, H2S SIBO/ISO, IBS, IBD, gastritis, GERD, H pylori, diverticulitis, candida, etc.) or have an autoimmune disease and need some help, I see individual clients to help them resolve their digestive issues or reverse autoimmune disease naturally, You’re welcome to set up a free, 30-minute breakthrough session to see if you’d like to work with me. I also have my own two products, Tributyrin-Max, which is particularly helpful for loose stool and diarrhea as it slows your motility and firms up your stool, and SBI powder, which is an all around gut pathogen binder, which is super safe and won’t harm beneficial bacteria, and is usually the first line of treatment I educate my clients about in order to avoid stronger antimicrobial herbs.

*Product and dispensary links are affiliate links for which I’ll receive a commission. Thanks for your support of the podcast by using these links. As an Amazon Associate, I earn from qualifying purchases.

